Briefing you on the latest in reproductive health research
TL/DR: Here’s what’s new in reproductive health research as of November 2020: Two COVID-19 vaccine candidates have emerged with encouraging new data; studies of symptomatic pregnant people with COVID-19 are concerning for the health of parent and child; a new treatment for endometrial cancer has finished a phase 1 efficacy trial.
Last month, we at Flex® introduced our new blog series, Updates in Period Health Research, to give our readers a quick monthly roundup of the news, stats, and advancements impacting the industry right now.
This month’s update is heavy on COVID-19, referencing the news that has been all over our feeds lately along with new research on COVID-19 in pregnant people.
A new drug for the treatment of endometrial cancer is also discussed, adding to our running list of emerging reproductive health treatments to watch in the coming months.
Not repro health-specific, but still a super important update: COVID-19 vaccine trials
PFIZER VACCINE CANDIDATE: 90% EFFECTIVE
On November 10th, the world woke up to a dose of optimism when Pfizer announced results from their COVID-19 vaccine study indicating it could be 90% effective.1 The candidate vaccine, which is a collaboration between Pfizer and German company BioNTech, is a two-dose schedule vaccine, meaning that anyone who gets it will have to receive the vaccine on two different occasions (with a set period of time in between the first and second dose).
The Pfizer study enrolled over 40,000 people. Of this group, 40% of global participants and 30% of U.S. participants were identified as racially/ethnically diverse. Notably, the vaccine was shown to prevent COVID-19 infection in those who had no previous exposure to the virus. Phase 3 of this study has been in progress since late July; this is the final stage needed prior to FDA approval and distribution.
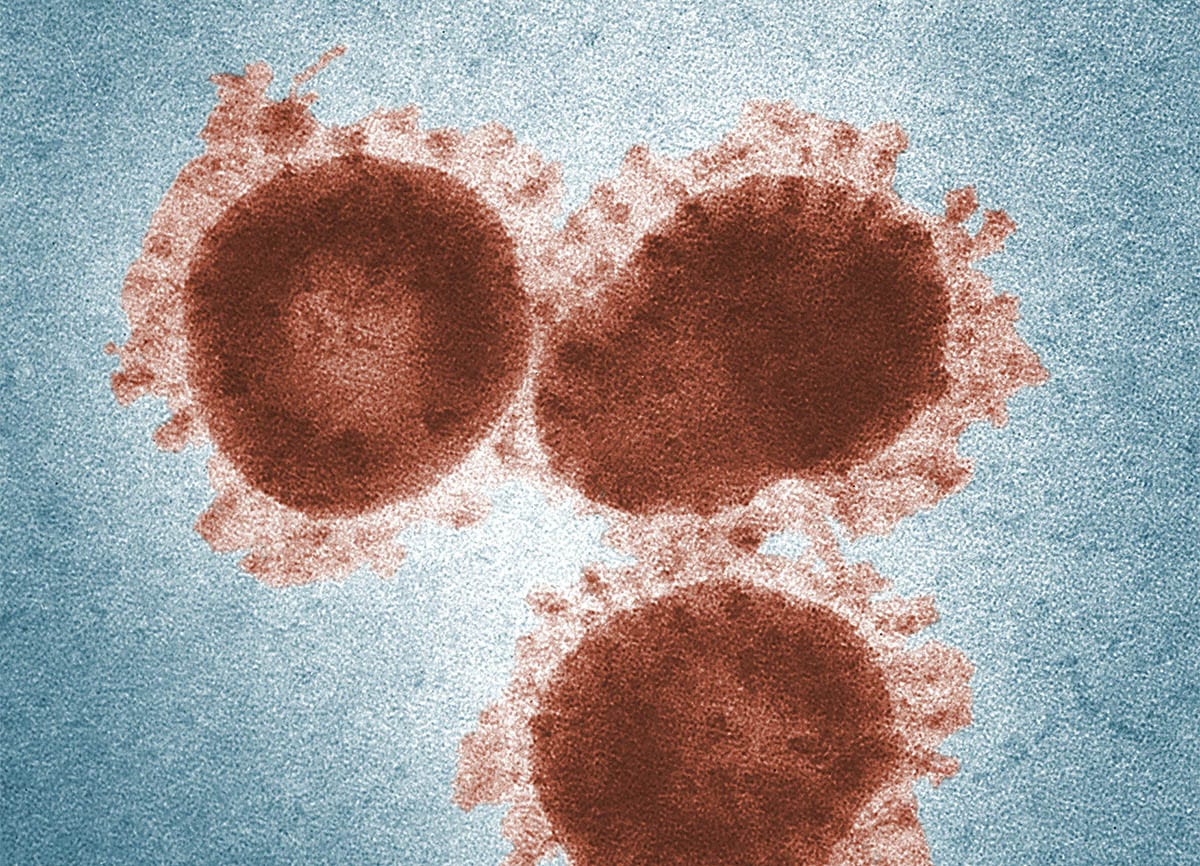
If you’re wondering how it’s possible to confirm the results of a study like this while the pandemic is still in full swing, you’re not alone. Because this strain of coronavirus is so deadly, vaccine researchers have been working double time to accelerate research and development. In some cases, vaccine companies that previously focused on another clinical area have switched to infectious diseases to meet the demand.
MODERNA VACCINE CANDIDATE: 94.5% EFFECTIVE
Not to be outdone, Moderna released initial results from their vaccine study just one week after Pfizer: They announced a preliminary vaccine efficacy of 94.5%.2 The Moderna study is similar to Pfizer’s, with a sample size of around 30,000, a two-dose vaccine schedule, 95 total COVID cases in the study, and about one-third of participants identifying as people of color.
Moderna’s study also had around 40% of its population coming from high-risk groups, like people with diabetes, heart disease, and obesity. This is incredibly important, as we know that people in these groups are at the highest risk of severe COVID-19 disease and/or complications.
All in all, this is cautiously good news for the global battle against COVID-19, if the data holds up. Both companies have indicated that they are prepared to begin producing their respective vaccines as soon as this year, with distribution projected for 2021.
However, it is important to address a huge caveat here: even if all goes according to plan, there will be a number of administrative and regulatory hoops to jump through to ensure that the vaccine is truly effective and, above all, safe. In the best case scenario, it will be months or longer before there is any widespread distribution of the vaccine.
This brings us to a super important takeaway: Don’t let your guard down now just because of the good news about vaccines. Keep that mask on, wash your hands, sanitize frequently, and stay physically distanced. The winter surge is here – and there are still millions of lives to protect.
New study explores COVID-19’s effect on health outcomes of pregnant individuals
Pregnancy during COVID-19 is a question that many experts have been ruminating on in recent months. Earlier this month, we explored how expecting pregnant people are coping during the pandemic in an interview with certified doula Jessie Laurore. Now, there is more data from ongoing studies updating the science behind what we know about pregnancy and this virus.
In a surveillance study done by the CDC, pregnant people with confirmed COVID-19 infection who were symptomatic were more likely to be admitted to the hospital during their first or second trimester, e.g. earlier on in the pregnancy.3 What were these admissions for? The data showed that these symptomatic pregnant people were more likely to be admitted for COVID-19 related reasons than for labor and delivery.
More on this: 16% of study participants were eventually moved to the intensive care unit and 8.5% required mechanical ventilation, which is concerning for the health of both parent and child. 25% of symptomatic pregnancies were also premature, which again raises the child’s risk for a host of health issues.
These findings aren’t entirely shocking (though they may be anxiety-inducing). Pregnant people are thought to be more at risk for respiratory viruses in general; so far, this holds true for COVID-19. This study also supports earlier data suggesting that pregnant people are more at risk for severe COVID-19 disease and premature delivery.
Although we still need to see more research on the topic, it’s fair to say that early identification of COVID-19 in all people, and perhaps especially for pregnant people, is key for the most successful diagnosis and health outcomes.
Hope for endometrial cancer treatments
Not to sound like a broken record here, but reproductive health conditions are still under-funded and under-researched. So, when we see new studies with promising results, we get pretty excited. This is one of those moments:
A new paper was released with results from a Phase 1 study of a monoclonal antibodyMonoclonal antibodies are blood proteins made in a lab that mimic your natural antibodies (the things that help you fight off foreign invaders like viruses, fungi, and bacteria). These antibodies can then go on to do many things, from stopping cell growth to blocking viral particles from entering your cells. called dostarlimab (no worries, we couldn’t pronounce it, either). It’s an antibody that’s shown promise in the treatment of endometrial cancer4, a condition in which cells in the lining of the uterus become cancerous, leading to symptoms like pelvic pain and bleeding between periods.5
Current treatment for endometrial cancer includes options like surgery, chemotherapy, and radiation depending on the extent of the cancer progression. However, treatment gaps persist for certain types of endometrial cancer – many are resistant to treatment.
To give you some more background info, phase 1 studies are designed to test potential treatments for safety and must be done prior to larger scale studies. In this specific study, about 100 women-identified patients with deficient mismatch mutation repair endometrial cancers (a.k.a. having cells with DNA mutations that tend to lead to cancer) were enrolled and treated with the experimental drug dostarlimab.
Here were their results: The confirmed objective response rate (a scientific term for the effect that the treatment had on cancer cells) was 42%, with an estimated 96.4% likelihood of maintaining this response at 6 months.
The researchers also noted that this was a clinically meaningful response, meaning that there was actually a reported benefit in taking the drug for these patients with endometrial cancer. Given the relative lack of reproductive studies for people with uteruses, especially in endometriosis and endometrium-related conditions, this will be an interesting one to watch in the coming months.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2021 The Flex Company. All Rights Reserved.