Understanding the hidden pain of endometriosis
TL/DR: Endometriosis affects nearly 200 million people worldwide, and it can take almost a decade to be diagnosed. Untreated, endo leads to period pain, irregular periods, and in severe cases, even infertility. Endo both affects your period and is affected by your period — and here’s why.
Last month, Olympic skater extraordinaire Tara Lipinski made waves when she posted on Instagram about her struggle with endometriosis. She invited fans into her hospital room with a series of powerful photos depicting her medical journey with the disease. She opened up about the intermittent pain that she felt for years. She also revealed how it wasn’t until recently that she sought out medical treatment for her symptoms.
Tara wasn’t alone in waiting for a diagnosis. The average delay to diagnosis – the time between noticing symptoms and getting an endometriosis diagnosis from your doctor – is 6.7 years.1 For some, that can mean nearly a decade of at-times debilitating symptoms. Some women start suffering from endometriosis in their teens and may suffer even longer times to diagnosis.
Endometriosis affects around 1 in 10 individuals assigned female at birth and of reproductive age. Regardless of this statistic, it is sorely underfunded in research dollars and not talked about nearly enough.2 Here’s the long and the short about endo and how it affects your period.
What is endometriosis?
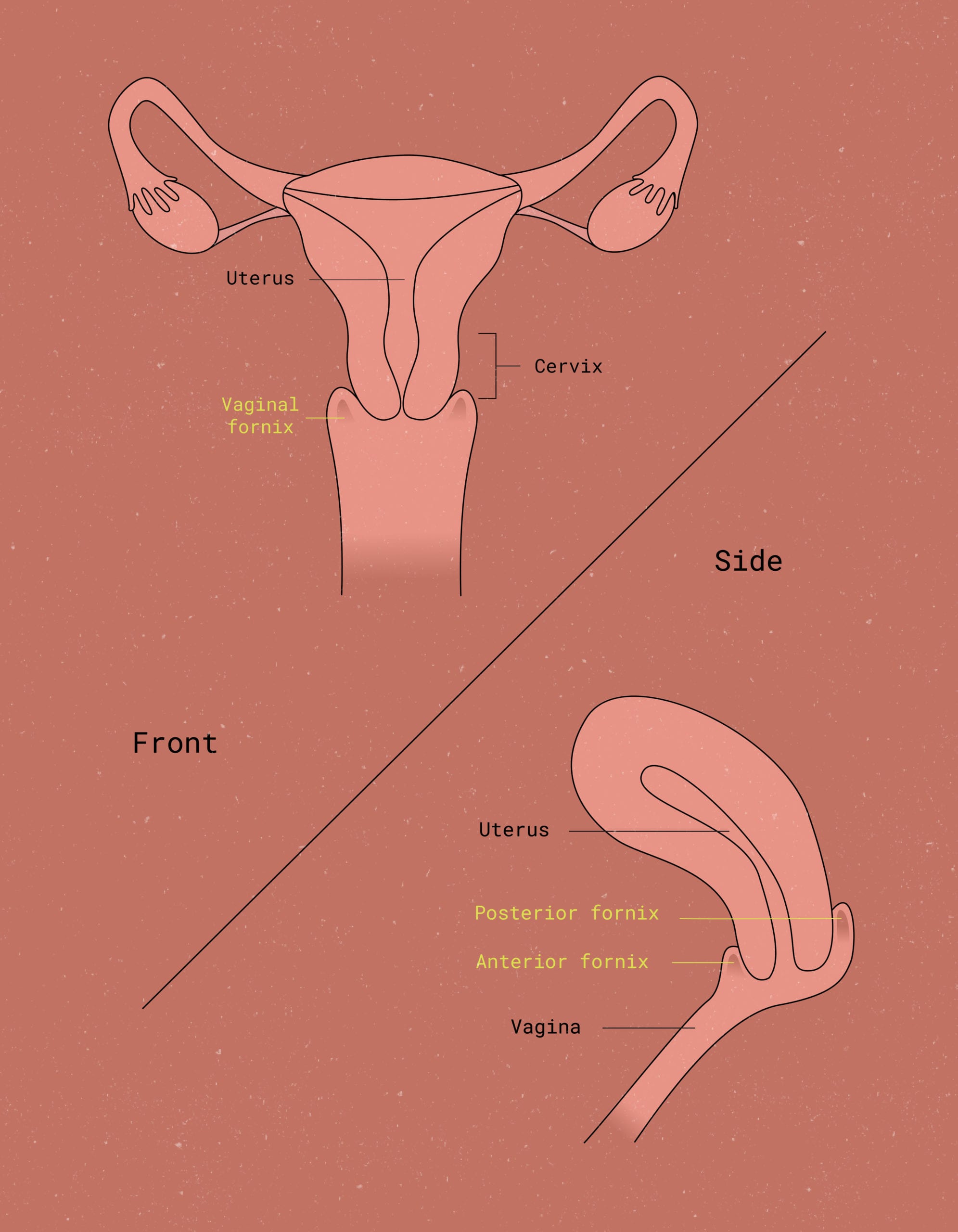
To understand what’s happening in endometriosis, first try to visualize the female reproductive system in all its glory. The vaginal canal leads up to the cervix, which is the gateway to the uterus. The uterus is a T-shaped structure that serves as the center for menstruation and reproduction. The lining of the uterus is called the endometrium – and it plays a key role during the menstrual cycle.3
During a typical menstrual cycle, the nutrient-rich endometrium builds up over the first couple of weeks of your cycle. Based on signaling from FSH (follicle stimulating hormone) and estrogen levels from your ovary, the endometrium thickens (or becomes vascularized) with nutrient-rich blood. Basically, it’s preparing itself to be a warm, wet, comfy home for the fertilized egg in the event of a pregnancy.
Then, ovulation happens – ta da! A brand-new egg is released by the ovaries. If that egg is fertilized by sperm, the endometrium will continue to build its lining. If the egg remains unfertilized, the endometrium will enter what is known as the secretory phase. During this time (the ~2 weeks before your period), the endometrium stops thickening and instead begins to secrete stored glucose.
It’s during the menstrual phase of your cycle that the endometrium really takes center stage. Hormonal signaling triggers those familiar uterine cramps that allow your body to shed the endometrium. That’s what brings about the bleeding that we all recognize as our period.
So: Endometriosis obviously has something to do with the endometrium – but what, exactly, is it?
Endometriosis is a condition in which endometrial-like tissue, begins to grow outside of the uterus. In most cases, this out-of-place tissue is found somewhere in the lower abdomen, or pelvis. However, it can technically appear anywhere in the body (brain, skin and lungs for instance). A few different hypotheses exist to explain why this might happen:4
What exactly is the cause of endometriosis?
Meyer’s Theory
suggests that endometrial cells become mutated, either spontaneously or through a genetic condition. This would allow these cells to grow without limits, resulting in the growths or polyps often seen with endometriosis. This explanation makes sense in theory, but it doesn’t explain how the endometrial cells move to where they’re found.
Sampson’s Theory
Suggests that endometriosis is due to retrograde menstruation. A “backflow” of menstrual blood during your period (not quite Mercury retrograde, but still not a positive thing). It’s thought that some of the endometrial cells shed during your period might travel out through the fallopian tubes and into the abdomen. This is the opposite direction that they’re supposed to.
Again, this theory sounds compelling in terms of its explanation as to how these cells end up outside of the uterus. However, 70-90% of menstruators experience retrograde menstruation, but only 3-10% of menstruators are diagnosed with endometriosis.5
Halban’s Theory
Provides an alternative explanation for cell spread. It argues that the endometrial cells move to distant parts of the body through lymphatics. Lymphatics are tunnels that exist all over your body through which your immune cells travel.
This theory could potentially make sense for the strange, distant sites of endometriosis polyps. However, it doesn’t explain why endometrial cells would also end up local to the uterus.
From these theories, we can learn that, at this point, we really don’t know what causes endometriosis. It definitely warrants further research (hello, Congress!).

How does endometriosis affect the menstrual cycle?
As previously mentioned, the endometrium is highly responsive to hormones, which makes sense for its role in menstruation and reproduction.2 But when endometrial-like tissue grows and spreads outside of the uterus,it can result in painful symptoms and ovarian cysts called endometriomas. These signs of endometriosis may last for years without treatment.
The endometrium is like your ovaries’ sidekick. When the ovaries say “Estrogen!” the endometrium says, “How thick?” When the ovaries say “Progesterone!” the endometrium is already scrambling to let out that stored glucose and eventually slough off the lining.
But when endometrial cells grow outside of the uterus, like in the fallopian tubes or ovaries, it can cause serious problems. It can lead to bleeding, scarring, and bands of scar tissue from endometriosis lesions called adhesions.
This whole process is responsible for the symptoms that many endo patients experience. Patients with endometriosis often experience heavy menstrual bleeding and/or irregular periods.6 Periods may also last longer since there is more tissue to slough off; some individuals even experience bleeding in between periods.
If you have an irregular period, speak with your healthcare provider, even if you don’t have any other symptoms.
Endometriosis symptoms: Period pain & irregular cycles
For patients with endometriosis, pain is the common thread. Many individuals diagnosed with endo experience pelvic pain, abdominal pain, period pain, pain during bowel movements and pain during sex.6 However, it’s important to remember that each person’s experience with endometriosis will be highly individualized.
Endo pain can vary significantly from one person to another. People can experience differences in severity, location, time of the month when it’s most noticeable, and how it changes over time.

In certain severe cases, endometriosis can also affect the reproductive organs and lead to a higher risk of infertility by causing the formation of scar tissue in the fallopian tubes. If you experience any of the below symptoms, consider reaching out to your healthcare provider for support.
- Heavy periods (i.e. bleeding that forces you to change your preferred form of period protection every two hours or less, bleeding that lasts longer than 7 days, or menstrual flow that involves clots larger than the size of a quarter)7
- Painful periods, including uterine cramps and cramps outside of the pelvis (e.g. lower back, stomach, rectum, upper legs, etc)
- Pain with sexual intercourse
- Severe bloating (A.K.A endo belly) that is painful and lasts longer than regular pre-menstrual bloating. Symptoms of endometriosis belly can also trigger physical, mental, and emotional symptoms.
- Severe pain in the pelvic area
- Nausea, vomiting, fatigue, diarrhea, bloating, etc., either on or around your menstrual period
How is Endometriosis Diagnosed?
Among other questions, your doctor will likely ask you what’s the area of pain and when it happens. This will provide initial information to detect endometriosis or other causes of pelvic discomfort.
There are many tests to check for endo, as you can see below:
Pelvic exam.
During a pelvic exam, your health care provider will check your pelvis for any palpable irregularities, e.g. endometrial cysts or scars behind your uterus. A limitation of this test is that unless a cyst has formed, small spots may be hard to detect in the pelvic cavity with just a physical exam.
Ultrasound.
Whether abdominal or transvaginal, an ultrasound test might be a good way to get a clearer look at your reproductive organs. While a standard ultrasound won’t confirm the diagnosis, it can detect endometrial cysts (endometriomas) connected with it. Endometriomas are ovarian cystic lesions.
Magnetic resonance imaging (MRI).
With an MRI exam, your doctor can get detailed images of your organs and tissues. Additionally, these images can provide specific info on areas of the growths’ position and size. This info can help your doctor if planning an endometriosis surgery.

Laparoscopy.
Additionally, your doctor may need to perform a surgical procedure called laparoscopy, for endometriosis diagnosis.
For this type of surgery, you must first be under general anesthesia. The surgeon will then make a small incision near your navel. After this, the surgeon will insert a laparoscope through the small cut, to look for signs of endometrial tissue outside the uterus.
Laparoscopic surgery is the preferred way to locate, measure, and diagnose, through visualization or biopsy, endometrial implants. With proper planning, the doctor can remove the endometrial cysts at this time. Through laparoscopy, your doctor can confirm the diagnosis and provide treatment for endometriosis, all in one procedure.
What are the treatment options for endometriosis?
Treatment options for endometriosis include pain management with medications, hormone therapy to reduce or eliminate menstrual periods, and surgery to remove endo implants. In severe cases, a hysterectomy may be considered as a last resort option to relieve symptoms.
Living with endo: Tips & strategies
There is currently no cure for it. It’s no wonder, therefore, that an endometriosis diagnosis can be devastating. Your doctor may recommend you treatment options or endometriosis medication geared towards pain relief.
However, no treatment is guaranteed to be 100% effective, and many entail long-term side effects. We recommend doing plenty of research before committing to a plan. If you plan to have a pregnancy, you may want to include an OBGYN or an OBGYN specialist to cover Reproductive Medicine, such as an Endocrine and Infertility doctor in your conversation.
The good thing is, if you’ve joined the ranks of endo warriors around the globe, you’re not alone.
Living with endo is best explained by those who know it best: the patients themselves. Padma Lakshmi, the chef, model, and activist, co-founded The Endometriosis Foundation of America alongside her gynecologic surgeon in 2009. This foundation aims to be a resource for patients seeking support.
There are also a number of online and (pre-COVID) in-person support groups. some of these groups are rooted in traditional, allopathic medicine, and others are more closely tied to integrative or holistic wellness.
Choosing menstrual products that work for you, especially ones that can accommodate heavy bleeding, may help with symptom management. Self-care practices may also help with cramps (along with pain medications, if your doctor gives you the go-ahead).
Endometriosis pain is no joke – if you’re suffering, don’t go through it in silence. Try to fill in your close friends, family members, teachers, and employers about your condition. This can help down the road, so you can ask for downtime when you need it.
Whichever way you seek support through your endo journey, know that there is a community out there for you. Don’t be afraid to speak up for yourself and your pain: You should always feel empowered to seek the information, resources, and support that you deserve.