Why is my period so heavy? All about menorrhagia
Everything you need to know about abnormally heavy period bleeding
When it comes to getting your period, establishing what’s “normal” is a fine art: Every human body is as unique as a snowflake, and your period is no exception. Your period may show up irregularly (i.e. one cycle is 26 days long, the next is 32 days long) or the number of days you bleed may go up and down. The pain you experience in the days leading up to menstruation may also fluctuate throughout your life.
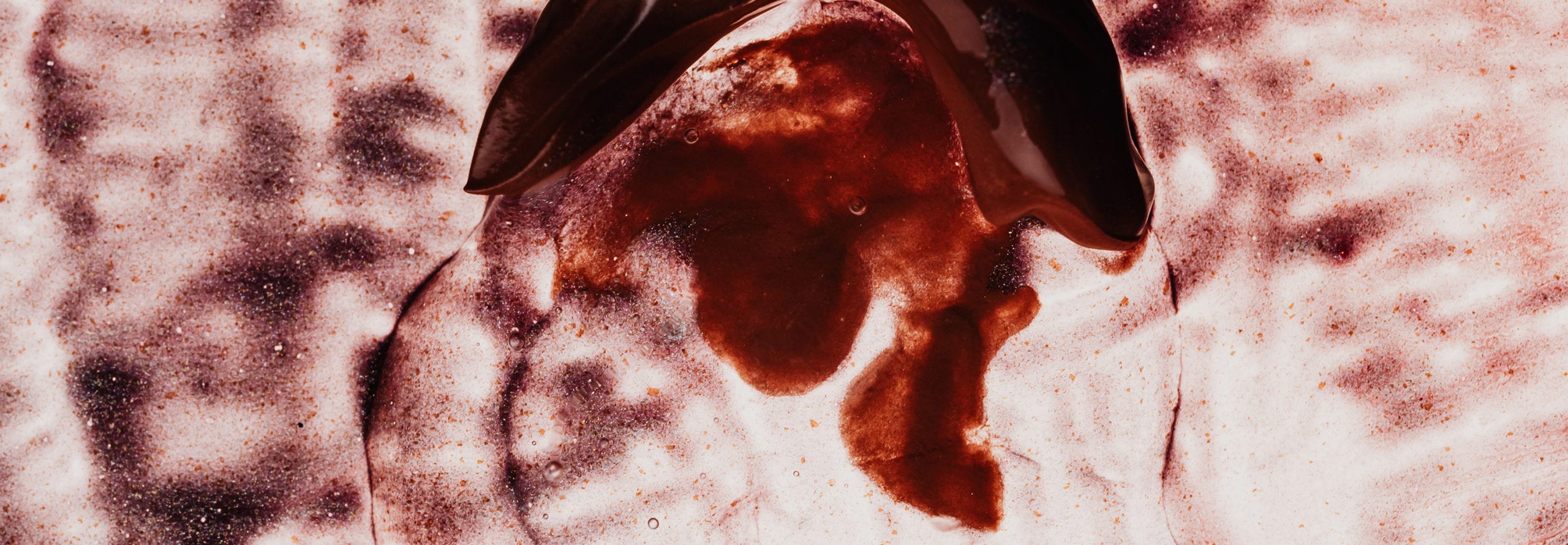
But one change we all tend to notice when it comes to our period is a sudden increase in the quantity of blood shed. Especially when it leads to unexpected leakage (always at the absolute worst moments, too). It’s annoying, concerning, and, TBH, straight-up disrespectful of your uterus.
For some, heavy periods are a temporary thing. They may be caused by a change in birth control, medication, or some other vague factor like an increase in stress. For others, a heavier period is just something they’ve always had and probably always will have, whether due to a chronic medical condition or just a genetic happenstance.
Usually, the only reason to worry is if your period is suddenly MUCH heavier than it’s always been. In these cases, make sure to talk to your doctor to investigate. In the meantime, we’ll explore some of the common causes of heavy periods (AKA menorrhagia) and offer up a few of our pro tips for coping with a heavy flow.
Menorrhagia definition: What is menorrhagia? And how much bleeding is too much?
A period usually lasts about 3-5 days and, on average, produces a total of 30-40 mL (6-8 teaspoons) of menstrual blood. The medical definition of menorrhagia is passing more than 80mL of menstrual fluid over the course of a period. This is more than double the “typical” amount.
These numbers are probably meaningless to you—unless you use a menstrual cup, in which you can see the actual volume of the blood you’re shedding. Even then, we’re guessing you’re probably not sitting on the toilet measuring out your blood like a goth scientist. So, if you’re not sure whether your periods are technically heavy or not, look out for these other signs:
- Large blood clots
- Bleeding through tampons in less than an hour
- Needing to double up on pads and tampons to prevent leaks
- Bleeding for longer than a week
- Blood flow so heavy that affects your daily life and you feel like you can’t manage it
Causes of menorrhagia (heavy periods)
Why is my period so heavy this month?!
You’ve asked it, so have we. Unfortunately, the answer is decidedly NOT simple: There are dozens of possible causes ranging from stress to fibroids to cancer.
If you’re freaking out about the worst-case scenario, don’t worry! Seriously. Heavy menstrual periods are a common medical complaint and, more often than not, menorrhagia is temporary.
If you end up visiting your doctor to discuss suddenly heavy or unusually painful periods (yes, this is a good idea!), keep in mind that a root cause is not clear in more than half of all reported cases. If you have other concerning symptoms, though, your provider will more easily be able to perform a differential diagnosis and get you started on the path towards treatment.
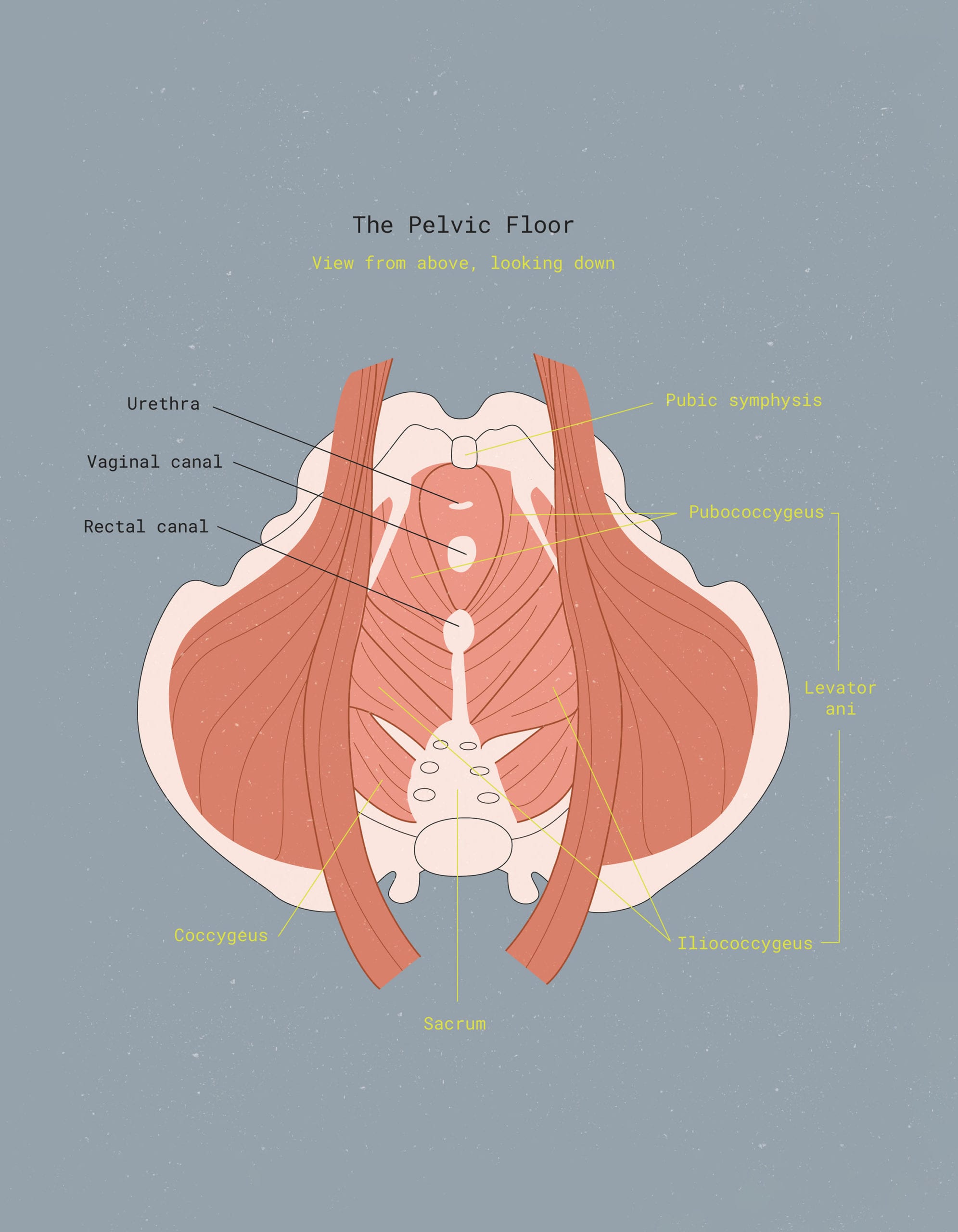
If you’re experiencing menorrhagia, your doctor or health practitioner may search for a cause with blood tests, a pelvic exam or ultrasound, or a hysteroscopy.
Here are just a few of the possible causes of menorrhagia:
Estrogen and progesterone imbalances:
These hormonal imbalances can cause buildup in the uterine lining. This will shed during a period, causing a heavier flow. Common conditions that could be linked to an imbalance in hormone levels include polycystic ovary syndrome (PCOS), insulin resistance, pre-diabetes, thyroid illnesses, hormone therapy, and obesity.
Endometriosis:
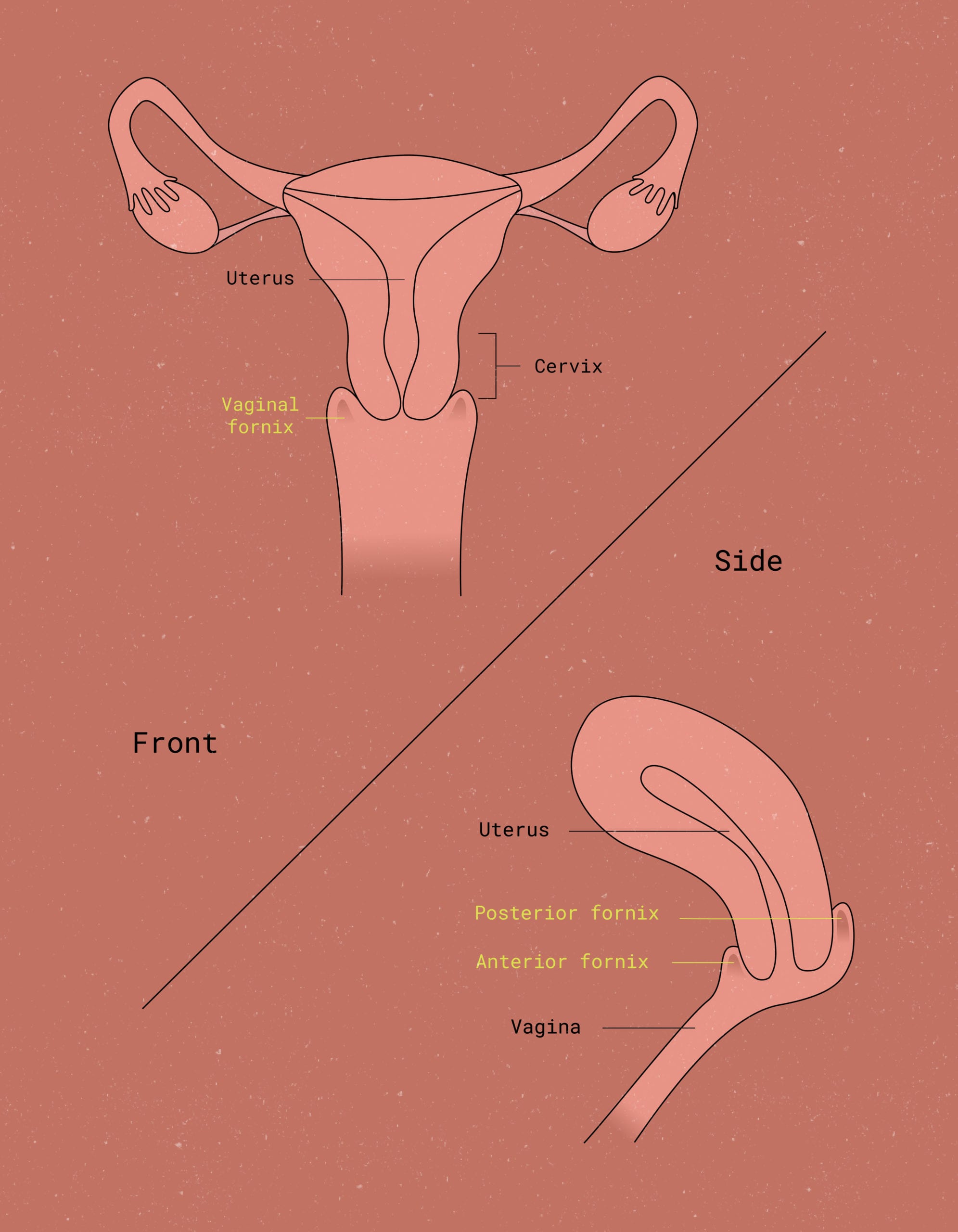
When uterine tissue grows outside of the womb and into other parts of the pelvic area, it can cause people with endometriosis to experience very heavy periods and cramping, and possibly clots in their period blood.
Polyps or fibroids:
Uterinepolyps are overgrowths of the endometrial tissue that lines the uterus and can be malignant, while uterine fibroids are (non-cancerous) growths in the actual muscle and fiber lining of the uterus. Some people are at greater risk for fibroids and polyps, so tell your doctor if your abnormal uterine bleeding comes with a family history of fibroids, polyps, or other uterine growths.
Adenomyosis (a.k.a. Endometriosis interna)
A condition in which glands from the endometrium become embedded in the walls of the uterus, leading to heavier or more painful periods.
Intrauterine Devices (IUDs):
Both the hormonal and non-hormonal IUDs may cause heavy bleeding. Heavy bleeding with an IUD is especially common in the first few months after insertion; the copper IUD is also more commonly known to cause heavy bleeding.
Pregnancy or miscarriage:
Pregnancy occasionally goes unnoticed before ending in a miscarriage, which can be mistaken for a heavier-than-normal period. An ectopic pregnancy can also cause heavy bleeding that could be confused with a period.
Cancers of the uterus and cervix:
These can cause heavy menstrual bleeding. But before you start panicking that your heavy bleeding = cancer, there are many other symptoms that are more reliable for a cancer diagnosis. Make sure you’re getting regular pap smears to ensure a healthy cervix.
Postpartum bleeding (Lochia):
Heavy vaginal bleeding after childbirth is common but it is not the same as getting a period. Postpartum bleeding can be dangerous if excessive and may be a sign of a hemorrhage.
Other bleeding disorders:
Various diseases can impair the body’s ability to coagulate blood, resulting in abnormal periods. People with Von Willebrand Disease, for example, are missing a blood-clotting protein and may experience menorrhagia.
Certain types of medications:
This includes aspirin and blood thinners (anticoagulants) such as Coumadin or Warfarin. Certain medications, including birth control, can also contribute to hormone imbalances that lead to heavy bleeding, or may impact clotting, which can also lead to increased bleeding.
Age:
Teenagers are more prone to heavy flow and irregular menstrual cycles in the year following menarche (your first period).
Perimenopause:
The years leading up to menopause (for some, that can last up to 10-15 years) is marked by heavy bleeding for many people.


Managing heavy periods
Making changes in your lifestyle can make heavy bleeding far more manageable. The following adjustments may help make your period more comfortable:
Diet and nutrition changes
If heavy period bleeding is causing you iron deficiency anaemia, certain foods, such as dark leafy vegetables, meat, fish, and tofu, can help make up for the blood loss, bump up red blood cells and restore healthy iron levels.
Regular exercise & active lifestyle
Regular exercise can help shorten your periods, reduce cramps, and lighten your menstrual flow by increasing your metabolism. It can also be a serious mood lift and stress-reliever. Don’t sweat how you sweat: If the gym isn’t your place, there are lots of other ways to get moving. Join a kickball league, sneak into the neighbor’s yard to take a dip in their pool, or go out to disco night at a roller-rink: voila, you’re exercising!
Medication for heavy menstrual bleeding
Hormonal types of contraceptives, such as birth control pills or a hormonal IUD, can help reduce the amount and duration of the bleeding. Aside from fighting inflammation, Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) such as Advil or Ibuprofen can also reduce menstrual blood loss and cramps. They can also increase bleeding, so ask your doctor if medication options are right for you.
Treatment for menorrhagia
Your provider will determine the best treatment options for you based on your unique health profile. These factors include your overall health, medical history, cause and severity of your menorrhagia, your future childbearing plans, as well as your opinion or personal preference. Available menorrhagia treatments range from medications like tranexamic acid to procedures like dilation and curettage (D&C) to endometrial ablation or even hysterectomy in the more extreme cases.
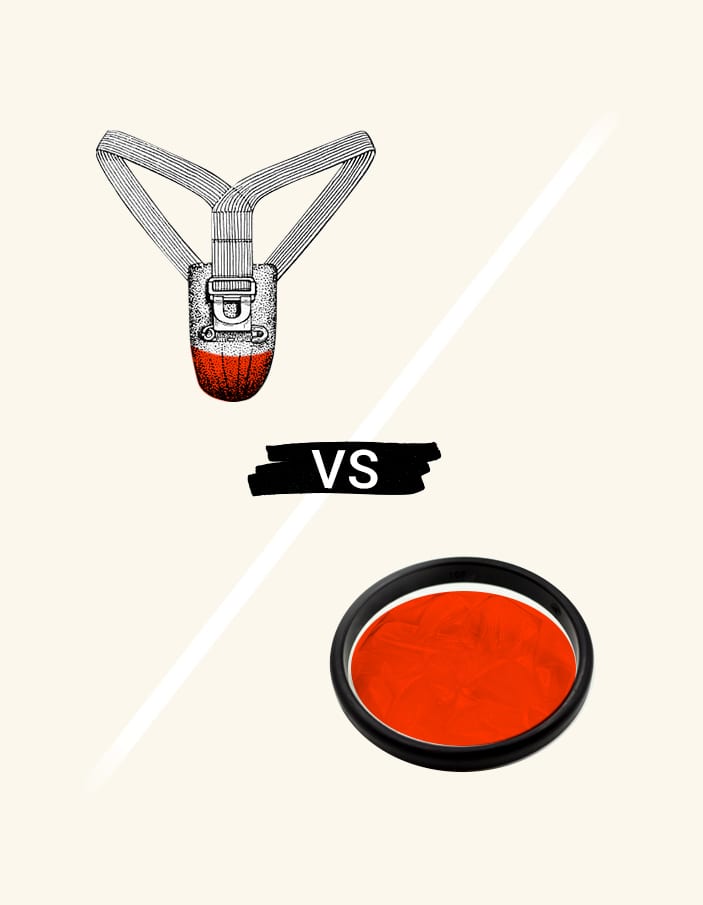
Menstrual products that help
If you are filling your pads and tampons faster than you can change them, consider switching to a menstrual product that can handle more blood. Menstrual discs and period cups both hold more fluid than tampons and pads (up to five times as much fluid!) and can stay inserted for up to 12 hours. Discs and cups can also reduce the cramping that goes with heavy bleeding, and they catch heavy period blood clots more effectively.


When in doubt: Go to thy doctor!
We love Googling “do I have cancer” at 2 AM just as much as the next person, but going to the doctor is truly your best bet for figuring out what, if any, implications there are with your heavy bleeding.
While menorrhagia is not necessarily a sign of an underlying condition, regular checkups with your gynecologist or primary care practitioner will keep an eye on anything that may be going on in your body. Be sure to talk with your doctor if you have any other conditions or symptoms in addition to heavy menstrual bleeding, as well as your family history.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2024 The Flex Company. All Rights Reserved.