Up close & personal with: Your pelvic floor
What does the Pelvic Floor do? What’s pelvic floor dysfunction?
What comes to mind when you hear the term, ‘pelvic floor?’ Some sort of geometric flooring pattern? Maybe an anatomy class you took (read: slept through) in high school? Or perhaps a mysterious, pelvis-adjacent body part?
If you chose option C, you’re correct. The floor of the pelvis is, indeed, a part of the body – and a pretty incredible one at that.
The pelvic floor refers to a set of muscles that we use practically all the time. Your pelvic floor impacts bathroom breaks, sexual sensation, childbirth, and even your ability to walk upright.
Since these layers of muscles play such a key role in the functioning of our digestive and reproductive systems, it’s not surprising that pelvic floor dysfunction (PFD) – when your pelvic muscles and ligaments aren’t quite functioning as they should – is so common, especially in individuals AFABAFAB stands for “assigned female at birth.”.
PFD affects 10% of uterus-havers between ages 20-39, 27% of those aged 40-59, and 37% of those aged 60-79.1
Clearly, this issue isn’t talked about enough. Luckily, we’ve found the fantastic physical therapists at Origin Physical Therapy in Los Angeles. They provide specialized physical therapy for women and mothers since 2007.
We spoke with Dr. Sarah Clampett, PT, DPT, Clinical Director at Origin, who filled us in on all the basics about the pelvic floor and what sort of issues can be addressed with pelvic floor physical therapy.
What is the pelvic floor
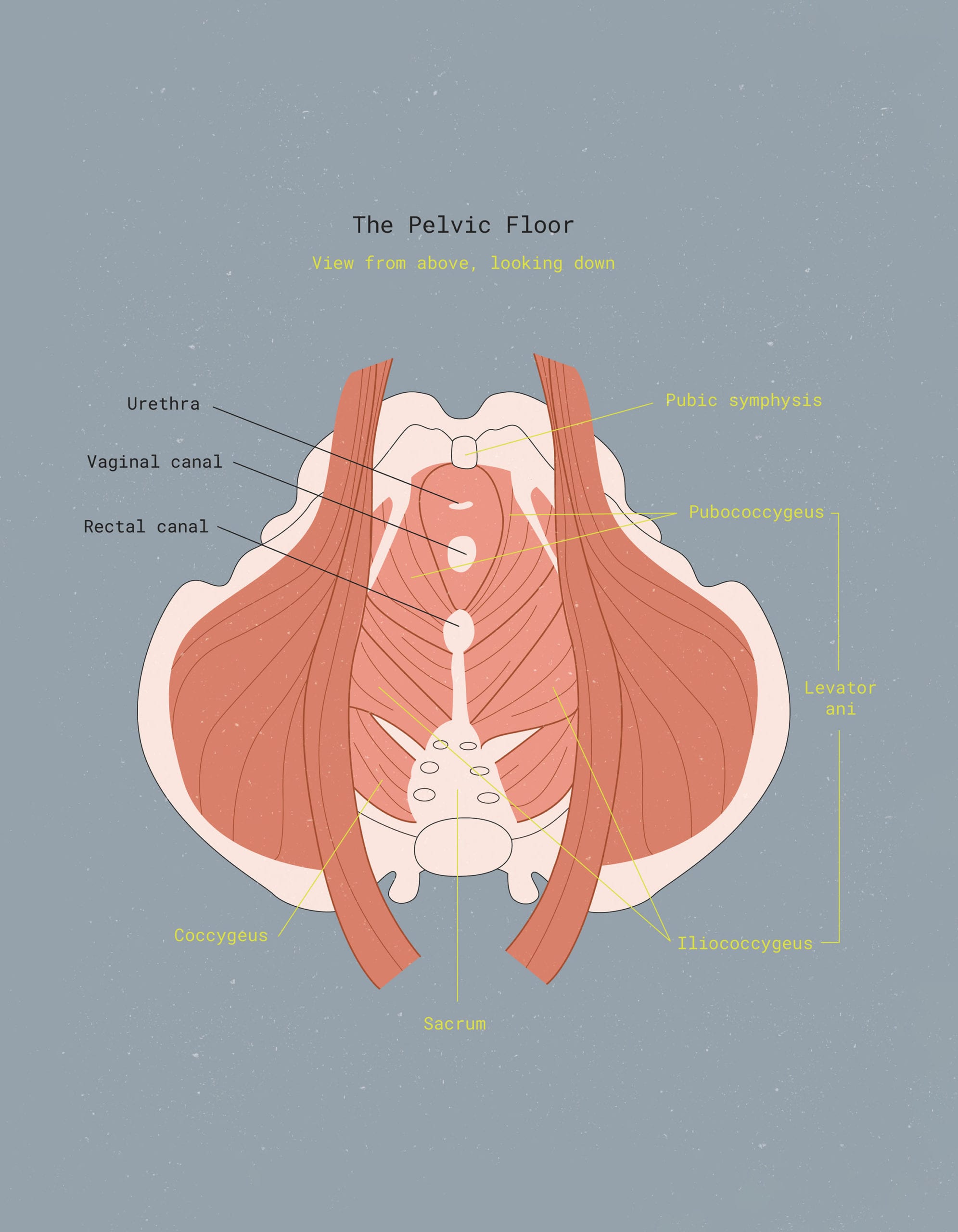
As you may have gathered by looking at the diagram above, the pelvic floor consists of several muscles with long, tough-to-pronounce names: pubococcygeus, puborectalis (not pictured), and iliococcygeus.
“The pelvic floor is a group of muscles that sit at the base of your pelvis like a bowl, quite literally like a floor,” explains Dr. Clampett. “It consists of three layers that work together to perform five major functions.” They are:
1. Support.
It directly supports the internal organs of the pelvis, which include your uterus, bladder and bowel function. It also supports pelvic organs against gravity and combats other pressures created in your belly (like a sneeze).
2. Continence.
The pelvic floor keeps you continent, meaning it keeps your urethral and anal sphincters tight and prevents the release of urine and faeces until you are ready to void. Without a strong pelvic floor, you may experience issues like urinary incontinence or fecal incontinence.
3. Stability.
Your pelvic muscles help stabilize your low back, hips, pubic bone, and pelvis, keeping your core strong and supported. These muscles contracting and relaxing to maintain a stable base for movement are crucial for overall body stability and balance.
4. Sexual function.
Your pelvic floor muscles are responsible for your sexual function and pleasure. During sexual intercourse, the pelvic muscles play a crucial role in sensation and orgasm. They help with arousal, vaginal tone, and overall sexual enjoyment.
5. Circulation.
Your pelvic floor muscles are known as a sump pump, meaning as they contract they pull fluid out of your abdomen and pelvis and send it back into your circulatory system, which decreases swelling and bloating in the pelvic and abdominal area.

What’s pelvic floor dysfunction (PFD)? What are the causes?
PFD is a condition that’s diagnosed based on your pelvic floor muscles and connective tissue not performing any one or more of the duties listed above.
“It can occur for many reasons, but most PFD is caused by the pelvic muscles being too tight, too weak, or a combination of both,” Dr. Clampett tells us.
Both tightness and weakness of the pelvic muscles tend to occur after childbirth or trauma to the region; these are two especially common causes of PFD. Other common causes include:
- Chronic constipation
- Hormonal changes (i.e. during puberty/menopause)
- Stress (!!!)
- Illness (particularly those with respiratory symptoms like coughing)
- Overtraining, especially high impact exercise
- Heavy lifting can also strain the pelvic muscles due to an increase in intra-abdominal pressure
- Injury to the surrounding joints or body parts (i.e. abdominal surgery or a hip injury)
- Smoking
- Obesity
What are the symptoms of pelvic floor dysfunction (PFD)?
Pelvic Floor Dysfunction symptoms can present in many different ways – it all depends on your unique medical history and the mechanism of the injury. However, the most common symptoms are:
- Pelvic heaviness or pelvic organ prolapse
- Urinary, fecal incontinence or difficulties with bowel movements
- Urgency to pee or overactive bladder
- Painful sex
- Perineal (the area of the body between the anus and the vulva in AFABAFAB stands for “assigned female at birth.”, and between the anus and the scrotum in AMABAMAB stands for “assigned male at birth.”) and/or pelvic pain
Pain from PFD can be intense, stretching from the vulva to the lower abdomen. It may feel like burning, stabbing, aching, or shooting pain, often accompanied by incontinence.
PFD is common in patients with Interstitial Cystitis, a condition known for chronic bladder pain and pain during urination.2
“More often than not, people with PFD will present with more than one symptom – i.e. painful sex and a feeling of pelvic heaviness,” says Dr. Clampett.
If you experience any of these symptoms, don’t ignore them. Consult your health care provider and consider contacting a pelvic floor specialist.

Treating Pelvic Floor Dysfunction: What are the options?
With proper and consistent treatment, PFD can be cured.
“Just like any other muscle group, the pelvic floor can be strengthened if it is weak or lengthened if it is tight. Furthermore, pelvic floor dysfunction CAN be fully resolved, but it is important that you know what is going on with your pelvic floor and that you are doing the correct exercises,” Dr. Clampett explains.
“If you do the wrong thing, meaning you are kegeling when your pelvic floor is too tight, it can make your symptoms worse and make it seem like pelvic floor exercises don’t work.”
It’s essential to note that experiencing urinary incontinence or pelvic pressure doesn’t always indicate weak pelvic floor muscles. Tight pelvic muscles can reduce flexibility, causing issues with contraction and coordination. It’s this lack of coordination that could be causing your incontinence and/or pelvic prolapse or heaviness. So, in that case, doing kegel exercises (squeezing those muscles for a few seconds and then relaxing) to strengthen your pelvic floor might not be recommended.
Here’s a helpful analogy: If your calf cramps during a run and causes ankle instability, doing heel raises won’t help. To relieve discomfort, try stretching your calf muscles.
When should you consider pelvic floor physical therapy?
Pain, incontinence, and unusual sensations in your pelvic region are never normal. Unfortunately, too many people tend to ignore the signs of PFD or are simply unaware that it’s treatable.
If you EVER feel like something is off with the way your pelvic floor functions, talk to your provider or consider seeing a pelvic health physiotherapist. Just because it is common doesn’t mean you should suffer through it.
“Something as major as childbirth or as minor as a cold can cause pelvic floor dysfunction,” Dr. Clampett adds. “With proper education and support, it can be improved and even resolved completely. Waiting to see if it will ‘go away on its own’ is never the answer.”
What’s the relationship between your pelvic floor muscles and period pain?
Period pain is caused by pelvic floor and abdominal muscle issues. Shedding the uterine lining leads to cramping and bleeding during menstruation. While some discomfort is normal, severe pain is not.
Pelvic floor PT can help to decrease the tone (tightness) and increase the relaxation and coordination of your pelvic muscles, providing some relief during menstruation.
PFPT can also make it easier to use certain period products that are worn internally, like tampons, menstrual cups, and menstrual discs. Why? Because you’ll be more easily able to relax your pelvic floor muscles during insertion, helping you get your product of choice properly placed inside your vaginal canal.
With removal, particularly for period products like the menstrual disc that require finger removal, being familiar with your anatomy simplifies and reduces mess during the process.

Can pelvic floor PT improve painful sex?
Painful sex is often the result of overactivity and poor coordination of your pelvic muscles. It can also occur after direct trauma, i.e. having a baby with or without a perineal tear.
If overactivity is the problem, the pelvic floor muscles can make intercourse painful because they’re simply too tight and inflexible. More pain leads to increased tightness, creating a vicious cycle that makes deep and prolonged penetration nearly impossible.
If trauma is the root cause, overactivity is often the longer-term side effect. Thankfully, pelvic floor PT can address the overactivity and poor coordination of the pelvic floor structure. PFPT can be a game changer, improving the quality of life for those suffering from painful sex.
“By creating length and mobility in the pelvic floor muscles, insertion and penetration can be pain-free,” Dr. Clampett notes. “Furthermore, in order to have an organism, your pelvic floor must contract and then relax. If you have difficulty with either, it can make sex less pleasurable and make orgasming difficult.”
If you experience pain or discomfort during sex or have trouble climaxing, your pelvic floor may be the cause. Consult your doctor or a pelvic floor physiotherapist for more information.
About Origin Physical Therapy
Founded in Los Angeles, California, Origin is a physical therapy platform that aims to bridge the care gap for women. It sets a new standard for pelvic healthcare, addresses gender bias in medicine, and provides physical therapy for over 40 million women with pelvic floor problems, reducing the need for surgeries and medical procedures.
At Origin, success is rooted in the belief that treating women requires a safe space and a whole body approach (that means your vagina and pelvic floor, too). Movement is medicine. Clinicians focus on patients’ unique goals and needs, providing expert guidance, targeted regular pelvic floor muscle exercise program, and strengthening.
Click here to learn more about Origin Physical Therapy.
© 2025 The Flex Company. All Rights Reserved.
- UChicago Medicine. (n.d.). Pelvic floor disorders. https://www.uchicagomedicine.org/conditions-services/pelvic-health/pelvic-floor-disorders[↩]
- Interstitial Cystitis Association. (2020, April 28). Pelvic floor dysfunction. https://www.ichelp.org/about-ic/associated-conditions/pelvic-floor-dysfunction/[↩]