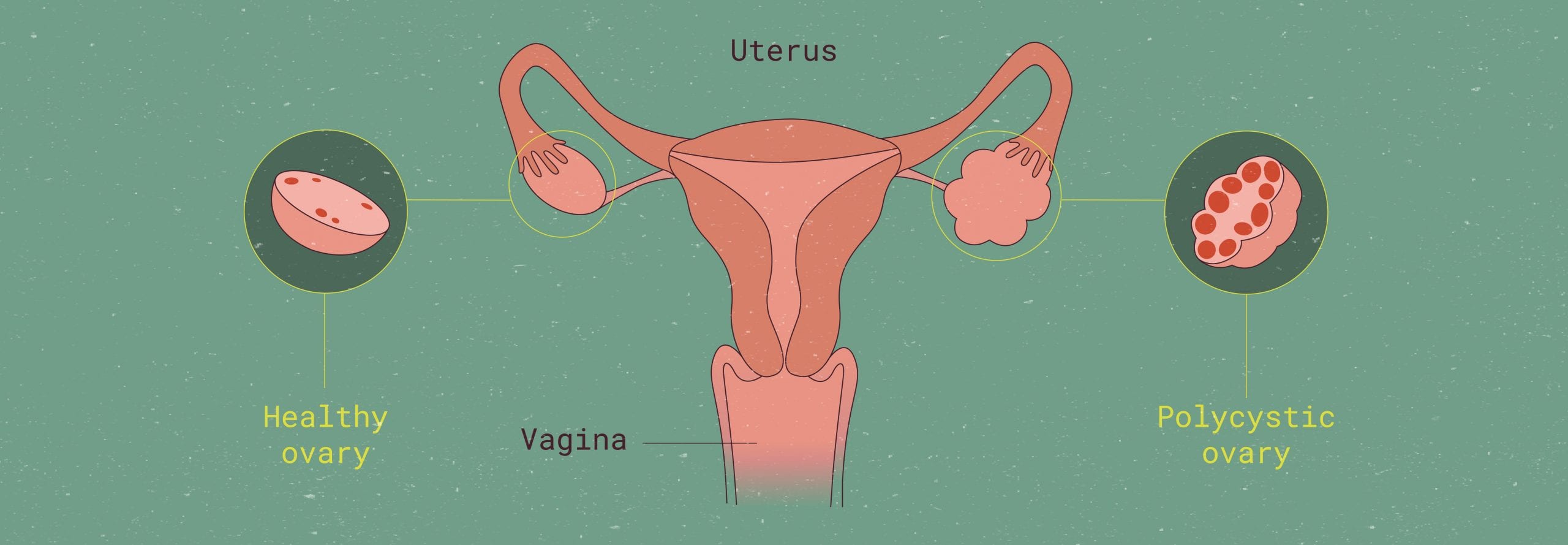
Comparison of normal ovary and polycystic ovary.
Guide to polycystic ovary syndrome (PCOS)
What is PCOS? Everything you need to know
TL/DR: PCOS stands for polycystic ovary syndrome. It’s one of the causes of irregular menstrual periods and can lead to fertility problems and other complications. Fortunately, PCOS is treatable. There are an array of medical options, as well as lifestyle modifications, that can help with PCOS symptoms.
Polycystic ovary syndrome (PCOS) is one of the most common endocrine disorders among people with uteruses, with an estimated prevalence (i.e. proportion of the population that is affected) that ranges from six to ten percent. 1
PCOS is a complex condition that is thought to be due to a combination of genetic and environmental factors. Hence, the name: PCOS. As a “syndrome”, it is characterized by a constellation of signs and symptoms that will vary from one person to another based on the unique interplay of their environment and family history.
Being a “syndrome” doesn’t mean PCOS is any less difficult or painful to deal with than other health conditions. And, for some, it can be frustratingly difficult to treat (and even more annoying to live with, especially during your period).
If you’re curious about what Polycystic Ovary Syndrome really entails or if you’ve been diagnosed with it, read on to learn more. We’ll cover how it is diagnosed, its most common symptoms, and how it affects your period.
How is PCOS diagnosed?
Polycystic Ovary Syndrome is diagnosed based on having two out of three criteria, which are:
- Infrequent or absent ovulation,
- hyperandrogenism (high levels of androgens),
- and/or the appearance of polycystic ovaries on ultrasound.2
Infrequent or Absent Ovulation
Infrequent or no ovulation at all is especially characteristic of PCOS. This is often one of the symptoms patients notice earlier on thanks to irregular or missing periods. In people with an regular menstrual cycle, ovulation happens roughly halfway in between the beginning of their menstrual periods. For those with Polycystic Ovary Syndrome, there are a few things going on that contribute to this failure to ovulate.
During ovulation, the ovary responds to hormonal stimulation and releases an egg, which is ready to be fertilized by a sperm. Follicles usually house the developing eggs, preparing them for release. However, for people with PCOS, there is a hormonal dysregulation that impedes follicular development. There is no fully developed follicle, no egg, and therefore no period.
Hyperandrogenism: Excess Androgens
Moving on to the second criterion when diagnosing Polycystic Ovary Syndrome: hyperandrogenism. This long, scary-looking word refers to the abovementioned hormonal dysregulation that prevents your body from properly developing an egg follicle.
So, what throws off hormonal normal levels? Individuals with Polycystic Ovary Syndrome tend to have excess androgens in their bloodstream, the result of higher levels of ovarian androgen secretion.
Androgens are steroid hormones that are present in biological males. They are also present in females, but to a lesser extent, they’re commonly referred to as “male hormones”. The main circulating androgen is testosterone.
Androgens are thought to be the culprit to certain other symptoms of PCOS. Physicians will run blood tests to check hormone levels as one of their first steps in diagnosing it.
The third criterion is the one that gives Polycystic Ovary Syndrome its name: the actual “polycystic-ness” of your ovaries. In simpler terms, it’s figuring out whether or not your ovaries have cysts dotting their surface. Cysts are sac-like pockets of tissue.
Polycystic Ovaries
The third criterion is the one that gives PCOS its name: the actual “polycystic-ness” of your ovaries. In simpler terms, it’s figuring out whether or not your ovaries have cysts dotting their surface. Cysts are sac-like pockets of tissue.
When follicular development is impaired, instead of one dominant follicle, several smaller follicles may form and fuse together, creating a cyst.
Your doctor might perform a pelvic exam to determine if your ovaries are enlarged. Ultrasound is usually the simplest way to get a visual of your ovaries. Ultrasounds are painless and widely accessible, offered at many outpatient practices and clinics.
According to the Rotterdam criteria, you need two out of the three “pieces of evidence” above to be diagnosed with PCOS. Keep in mind that these guidelines may differ depending on your healthcare provider.
Polycystic ovary syndrome: symptoms & how to deal
What are the symptoms of PCOS? Additionally to period irregularities, there are also other symptoms related to excess androgens in the bloodstream:3
- Menstrual irregularities, including infrequent or absent menstrual periods
- Menorrhagia, or heavy menstrual bleeding when there is a period
- Excess hair growth on regions such as the face, chest, and arms
- Acne
- Hair loss and/or male-pattern baldness
- Weight gain, obesity
- Insulin resistance, putting PCOS sufferers at higher risk for high blood sugar levels that can progress into type 2 diabetes
- Sleep apnea
- Difficulties becoming pregnant or infertility
Polycystic Ovary Syndrome and other conditions
Polycystic Ovary Syndrome has also been associated with chronic low-grade inflammation, which is thought to contribute to the long-term cardiovascular risks and complications associated with the condition. It’s important to note that not all PCOS sufferers will experience every symptom, and the severity of symptoms can vary from person to person.
PCOS sufferers are also at higher risk of developing health problems such as metabolic disorders such as high blood pressure, high cholesterol levels, heart disease, endometrial cancer, and non-alcoholic fatty liver disease.
Women with PCOS often notice the changes in their period early on, especially if they had a normal menstrual cycle. Some changes include: changes in number or length of the period, multiple missed periods without a pregnancy, or heavy menstrual bleeding.
You should always listen to your body and contact your health care provider whenever you notice changes in your menstrual cycle. If you have some of symptoms listed above, take note of them. Jot down dates and symptoms; that way, you’ll be armed with specifics when you bring it up to your provider.
Coping with PCOS symptoms: exercise, diet, and lifestyle adjustments
Managing PCOS can be difficult, especially as many of the symptoms are all-encompassing. The missed or irregular periods are stressful and the pelvic pain can be overwhelming when a period finally arrives. Not to mention the super-heavy bleeding and constant fear of leakage, even on “light” days.
Thankfully, there are many treatment options available to manage the condition. Therapeutics include certain hormonal birth control pills and fertility-boosting interventions for those struggling to conceive. Metformin, a drug that helps those with insulin resistance (which commonly occurs alongside PCOS) is also a treatment option.4
Since it is more common in individuals with high body weight, lifestyle changes can make a huge difference in reducing PCOS symptoms.
Polycystic Ovary Syndrome: Diet & Exercise
A customized PCOS diet and exercise routine can have a big impact in balancing hormone levels, reducing the severity of Polycystic Ovary Syndrome. A diet that is high in lean protein and low in fat and “empty” carbohydrates is a good place to start. Avoid white bread, french fries, candy, soda, and sweets.
There is no need to completely overhaul your diet or workout routine overnight. Take little steps, practice them consistently, and reward yourself for the progress you make.
The same goes for exercise. Get some extra steps in by parking your car at the back of the grocery store. Maybe take a walk instead of watching TV, or do a 10-minute YouTube workout class during your lunch break.
Some nutritionists recommend the DASH Diet for people with Polycystic Ovary Syndrome. This diet provides specific daily portion recommendations for various food groups to maximize cardiovascular health.5 However, finding a PCOS diet that works for you as an individual is key. A diet that helped a friend, parent or sibling lose weight might not work for you, and vice versa.
You can also keep a symptom diary to identify the lifestyle triggers that make your PCOS feel worse. You can include daily meals, exercise, sleep, and symptoms. Over time, you’ll start to pick up on certain patterns.
Gradual, sustained weight loss may help with the metabolic components of PCOS, like insulin resistance and high blood pressure. It may also improve other symptoms, like stubborn acne. If you can, try to work closely with a healthcare provider or nutritionist when creating a weight loss plan. Having someone’s support, helping monitor your progress and customizing your routine, will make it easier to maintain your results long-term.
Polycystic Ovary Syndrome & periods
The exact cause of PCOS is unknown, but it is believed to be caused by a hormonal imbalance that results in higher androgen levels impairing follicular development.1 Instead of one dominant follicle that supports the ovum, your body tries to develop multiple unsuccessful follicles.
These multiple follicles clump together in the ovary, forming polycystic ovaries. In PCOS, there can be more than 20 follicles found in the ovary at any given time.2 This decreased or even absent ovulation can eventually progress to infertility.
In the early stages of PCOS, people often notice changes in their menstrual cycle. Periods may also be shorter or longer than that person’s “norm”. The first period after a skip may also be heavier, as the uterus has more to shed.
Any irregularity in your menstrual cycle should be brought up with your healthcare provider ASAP.
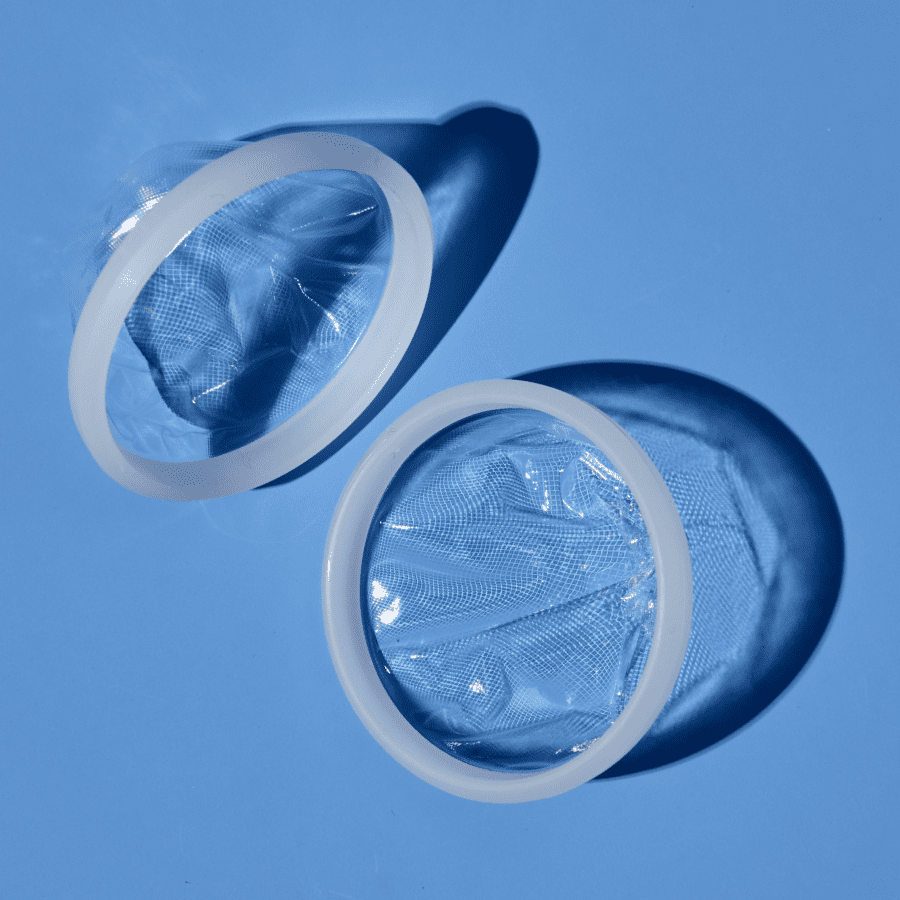
If you’re struggling with heavy periods as a result of Polycystic Ovary Syndrome, consider switching up your period product. Tampons and pads can only hold a maximum of 12-15 mL of fluid. Menstrual cups and discs, on the other hand, can hold up to 30 mL (about 6 teaspoons) of period blood.
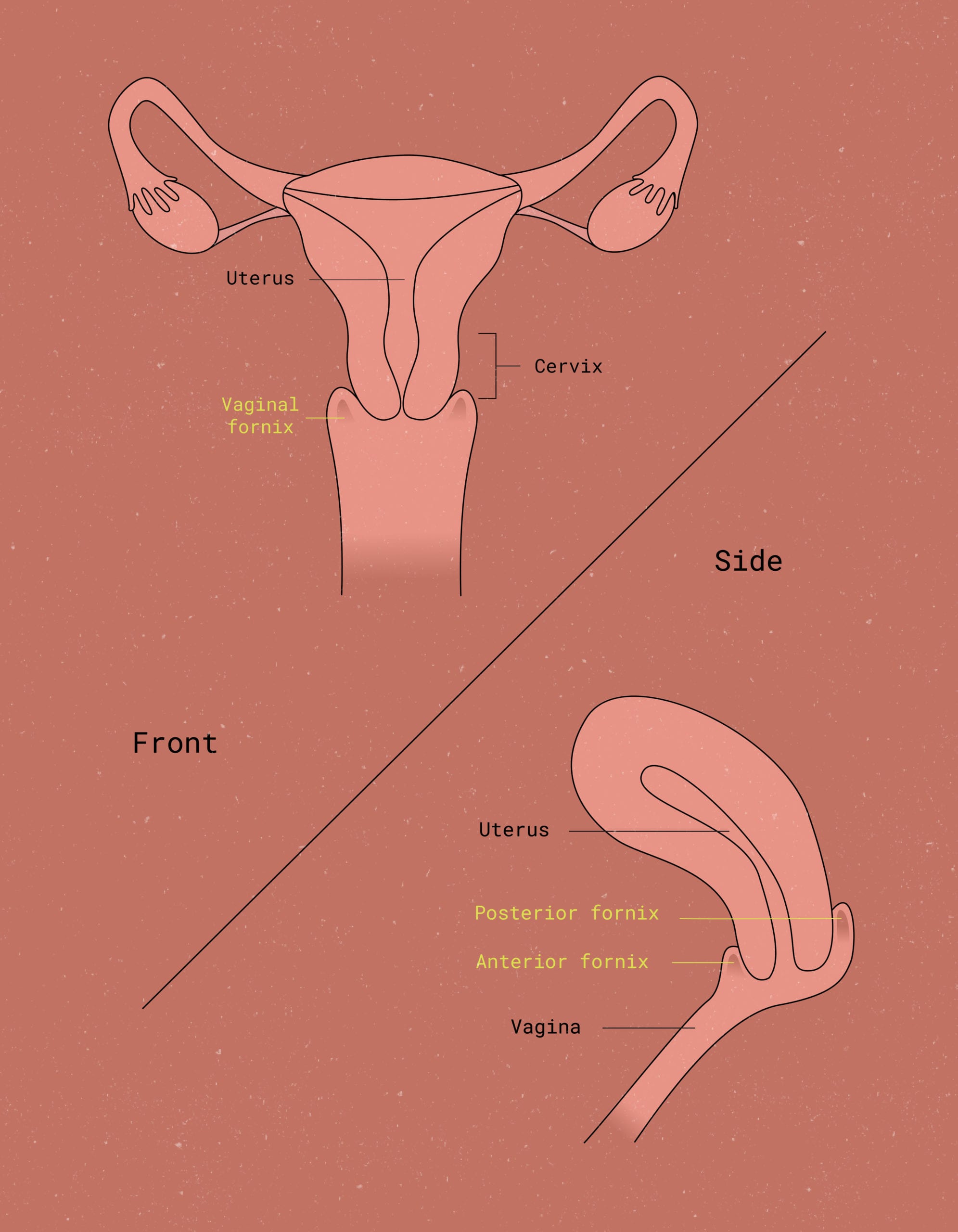
If cramps are a problem, menstrual discs like Flex Disc™ may also offer some relief. Discs sit in the widest part of the vaginal canal. Because of this, they don’t apply the same constant pressure to your vaginal walls that a tampon does.
PCOS & fertility
Polycystic Ovary Syndrome can impact the menstrual cycle, so it’s not surprising to learn that the condition can also impact fertility.
In people with PCOS, ovulation is irregular or, at times, completely dysfunctional (meaning there is no egg released from the ovary). Even when an egg is released, the reproductive milieu is impacted such that miscarriage rates are higher among people with Polycystic Ovary Syndrome.3 The miscarriage and infertility risks that come with PCOS can be a very heavy emotional burden for patients.
Fortunately, there are treatments that may help to regulate the menstrual symptoms of PCOS and thus regulate ovulation. These will usually take the form of combined estrogen-progestin oral contraceptives. Other options may be presented by your provider depending on your medical history.6 Consistent contraceptive therapy can help to restore the hormonal balance, leading to a more regular cycle.
Along with that, if you are interested in becoming pregnant, there are ovulation induction-type therapies available. It is possible to become pregnant with PCOS. An early diagnosis and commitment to treatment, alongside compassionate providers, are perhaps the best ways to boost your odds.
Polycystic Ovary Syndrome & mental health
Symptoms of PCOS can not only impact your physical health but also your mental health. It can be difficult to go through a painful and irregular menstrual cycle. Even more if its coupled with other symptoms – like acne, sleep apnea, and unexpected hair growth. It’s not surprising that PCOS brings with it a psychological burden.
If you struggle with PCOS, consider joining a peer support community that addresses both the mental and physical effects. Connect with others who understand your experience and ask your provider for recommendations.
If you have the resources, it may also be helpful to work with a therapist who specializes in chronic illness. The Psychology Today website has a fantastic search feature that allows you to look up therapists in your region. Plus, you can filter by specialty, accepted insurance, gender, and type of therapy. Many therapists accept sliding-scale pay or less expensive group sessions, both in-person and online.
Other tools and strategies that can help
On a different-but-related note, journaling is also an excellent tool for navigating chronic illness. Use it to track your symptoms and vent about them. Write about how you got through a particularly painful period, or strategies that made an immediate positive impact on your day.
Living with PCOS is challenging, but the symptoms are treatable. By identifying the signs early and seeking medical treatment, you can improve your outcome.
Key takeaways
- PCOS is an endocrine metabolic condition characterized by a hyperandrogenic state, irregular or absent ovulation, and the presence of polycystic ovaries on imaging
- PCOS symptoms are menstrual changes such as irregular periods. Also an array of symptoms that include excess hair growth, male pattern baldness, acne, and metabolic changes
- PCOS is completely treatable. Treatment includes hormonal medications otherwise known as oral contraceptives, certain therapeutics for insulin resistance, as well as supportive care
- Lifestyle changes like diet and exercise modifications can also help with the severity of symptoms
- Changing up your period product may be helpful for those with PCOS struggling with heavy or painful periods. Menstrual cups and menstrual discs hold up to 3x as much blood as pads or tampons
- Focusing on whole-body wellness is key for people experiencing PCOS
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2023 The Flex Company. All Rights Reserved.
- Azziz, R (2019). Epidemiology, phenotype, and genetics of the polycystic ovary syndrome in adults. UpToDate. Retrieved December 31, 2020 from https://www.uptodate.com/contents/epidemiology-phenotype-and-genetics-of-the-polycystic-ovary-syndrome-in-adults.[↩][↩]
- Barbieri RL & Ehrmann DA (2020). Diagnosis of polycystic ovary syndrome in adults. UpToDate. Retrieved December 31, 2020 from https://www.uptodate.com/contents/diagnosis-of-polycystic-ovary-syndrome-in-adults[↩][↩]
- Barbieri RL & Ehrmann DA (2020). Clinical manifestations of polycystic ovary syndrome in adults. UpToDate. Retrieved December 31, 2020 from https://www.uptodate.com/contents/clinical-manifestations-of-polycystic-ovary-syndrome-in-adults[↩][↩]
- NHS. (2017, October 20). Polycystic ovary syndrome – treatment. https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/treatment/[↩]
- Asemi, Z., & Esmaillzadeh, A. (2015). DASH diet, insulin resistance, and serum hs-CRP in polycystic ovary syndrome: a randomized controlled clinical trial. Hormone and Metabolic Research. 47(3), 232–238. https://doi.org/10.1055/s-0034-1376990[↩]
- Barbieri RL & Ehrmann DA (2020). Treatment of polycystic ovary syndrome in adults. UpToDate. Retrieved December 31, 2020 from https://www.uptodate.com/contents/treatment-of-polycystic-ovary-syndrome-in-adults[↩]