Re: Choosing the right menstrual products when you have an IUD
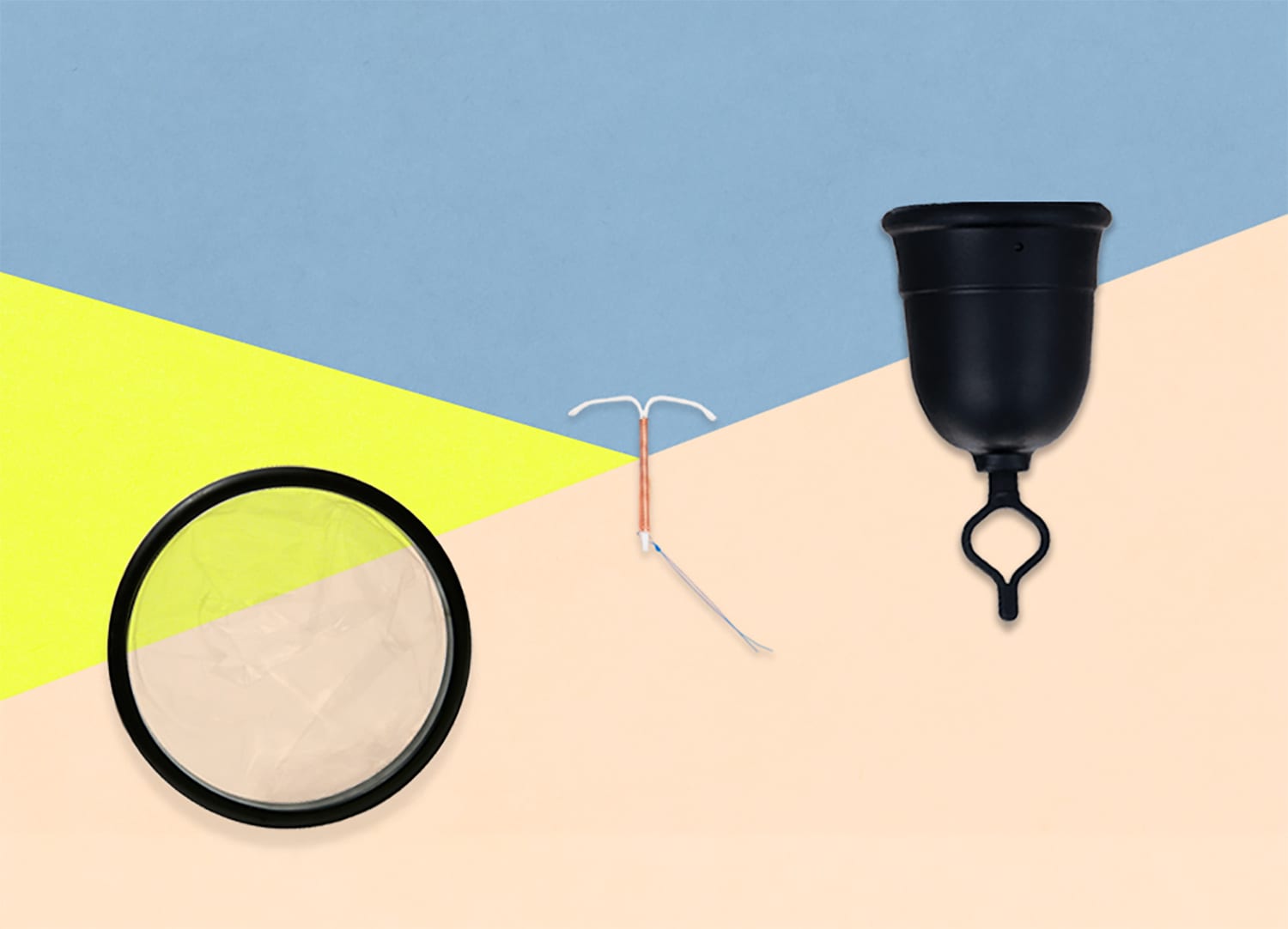
TL/DR: While it’s generally safe to use a menstrual cup or disc with an IUD, your risk for accidental IUD expulsion or displacement will depend on multiple factors. This includes whether you are using a disc or cup, the type of IUD you have, the position of your strings, and your unique anatomy. The best way to know for sure is to seek professional help.
Here’s a question we get asked a lot: “I’m thinking about getting an IUD and I’m worried about whether I’d be able to accidentally pull it out with a menstrual cup or disc – is that a thing that can happen?”
It’s a valid concern. Unfortunately, the answer is a little bit complicated and, thanks to the lack of scientific literature available, a little vague. So, we decided to dedicate a blog post to the topic with some up-to-date, research-based information on the safety of certain menstrual products for IUD users.
Keep in mind that this information is still changing. We’ll do our best to update content regularly as more studies are completed and more data is compiled. If you have a specific or urgent concern pertaining to your own IUD and menstrual product use, speak with your healthcare provider. When in doubt, get it checked out!
Learn more about accidental IUD expulsion and menstrual product safety.
What’s an IUD? And what’s it have to do with period products?
If you’ve heard of them before but you’re aren’t sure what we’re talking about–don’t worry. The term “IUD” is short for “intrauterine device.” It’s a form of birth control that’s become more popular in recent years.
Its popularity is because unlike the pill, patch or ring, it doesn’t require any sort of daily or weekly remembering. It just does its thing, hanging out in the uterus and preventing pregnancy for up to 5 years.
Different types of IUDs are available in the US and they fall into two categories. There’s the hormone-free copper IUD (i.e. ParaGard) and the hormonal IUD such as Mirena, Kyleena, Liletta, and Skyla.
Hormonal IUDs work by two methods: they alter the mucus on the cervix to make it thicker, thus preventing sperm from reaching any eggs. And they can prevent eggs from being released from the ovaries. This means that there is no egg to be fertilized by a sperm.
Copper IUDs work similarly to hormonal devices, but instead of releasing hormones to prevent pregnancy, it releases copper into the uterus. The copper alters the cervical mucus, which makes it more difficult for sperm to reach and fertilize eggs.
Which type you choose will depend on many factors. For example, whether you’re considering birth control as a way to mitigate heavy bleeding or to stop getting your period altogether.
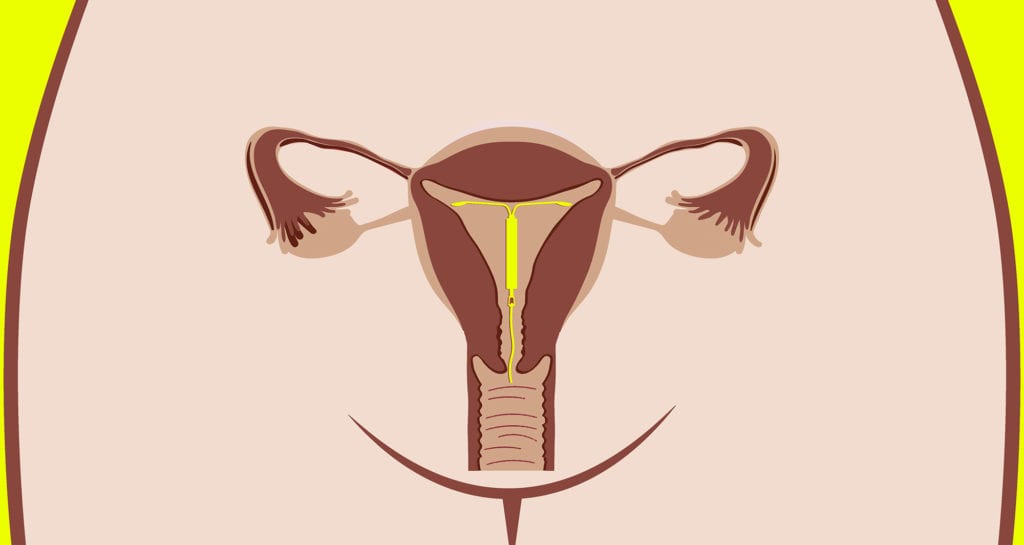
Why does the type of period product you use with an IUD even matter? Well, IUDs are placed in your uterus: They’re little, T-shaped devices, about the size of a quarter, that are inserted through the cervix (by a trained healthcare provider), and they have strings attached to the bottom. These strings exist so that your healthcare provider has something to grasp onto when it’s time to remove the device.
IUD strings come down through the cervix and hang slightly into the vaginal canal. How far down the strings hang depends on many factors, including the device, whether or the strings were trimmed, and your unique anatomy. In most cases, you won’t notice the strings unless you insert a finger up there to check on them.
There’s a slight risk that your device could be accidentally dislodged should something get caught on those strings. The device can be displaced even if a certain amount of suction is applied to the vaginal canal. While having something unexpectedly pulled out of your uterus through your cervix can be painful, there are women whose IUD falls out and they don’t know that it’s been expelled.
However, cases of accidental IUD displacement or expulsion are relatively uncommon.1 Read on to learn more.
IUD displacement & expulsion: The research
There aren’t a ton of studies out there on IUD expulsion (which is just a sciencey term for accidental removal) – and there appear to be even fewer on IUD displacement (which is when the IUD moves out of its proper position).
However, the research we do have shows that, on average, expulsion happens to roughly 6% of IUD users.1 Different factors appear to influence the likelihood of accidental expulsion – including menstrual cup use, as we’ll discuss in greater detail below – but the body of research is still too limited to make blanket statements about those factors.
In a 2012 study, for instance, “more expulsions were observed in females aged 14–19 compared to older women regardless of parity or IUD type.” in that same study, the researchers note in that “the higher incidence of expulsion observed among females aged 14–19 years should not discourage healthcare providers from recommending IUDs for this population.” They mention that, in most situations, the advantages of IUDs outweigh the risks.1
How does IUD displacement or expulsion happen if it’s not due to something getting caught on the strings? According to another 2016 study, “Incompatibility between the IUD and the endometrial cavity will provoke uterine contraction in an attempt to expel the IUD. These forces can compress, distort, displace, and expel the IUD, particularly if the IUD is not capable of adaptive changes.”2
In other words, if your device isn’t placed correctly (and even if it is), your uterus could contract and dispel it. Don’t freak out, though – this sort of displacement is rare.2
Menstrual cup & IUD: Can you use them together?
The short and simple answer here is yes. But that answer comes with a couple caveats.
While uncommon, there is always a risk of dislodging, displacing, or removing the device by pulling on the string while removing your menstrual cup (the same can happen during tampon removal).

The risk for IUD expulsion is affected by many factors. The same applies for the risk for menstrual cup-related expulsion:
- The position of your cervix
- How long it’s been since your intrauterine device was inserted
- The length and position of the strings
- The specific type or brand of menstrual cup you’re using
The only person who should really be telling you whether or not it’s safe to use IUDs and menstrual cups is your provider.
If you have any concerns about using a menstrual cup with an IUD, call your doctor or OB-GYN. You can also make an appointment with your local Planned Parenthood health center for a consultation or in-person visit.
If you’re looking for some facts and figures, keep reading. A recent 3-year study shed some light on the rate of IUD expulsion in menstrual cup users versus non-cup users:
All participants had a copper device placed at the beginning of the study. After one year had passed, the researchers found that IUD expulsion rates were 14.3% among menstrual cup users and 4.7% among non-cup users.3 By the end of the second year, these rates increased to 23.2% and 6.5%, respectively.
Keep in mind that this study only involved copper devices – so these rates do not necessarily apply to hormonal IUDs. And, authors suggest, that because hormonal devices often lessen the amount of bleeding and length of menses. Another term for menstrual flow (commonly known as your period)., the rates might be lower in those using a hormonal IUD because they will use menstrual cups less often.
What about the suction that holds the cup in place?
Could the suction that holds a menstrual cup in place be a blessing and a curse? Could the cup’s vacuum-tight seal accidentally displace your device during a hasty removal?
Researchers have wondered the same thing – and they’ve asserted that it’s especially important for IUD users to break the seal before removing a menstrual cup to avoid suction. Here’s a closer look:
A 2019 case series followed seven unique IUD expulsions that took place in patients ages 16 – 26. In all seven cases, expulsions occurred when patients were removing a menstrual cup. The researchers concluded that “there are two plausible mechanisms for IUD expulsion with menstrual cup use: (1) patients may unintentionally pull the IUD strings when removing the cup, and (2) the suction and vacuum created during cup application may dislodge the IUD.”4
They go on to offer a few words of advice for menstrual cup users with IUDs, recommending that they “break the cup seal prior to removal and [discuss] the option of cutting the IUD strings flush with the cervix as a potential way to reduce risk of expulsion.”4
Whether or not you have an IUD, you should always break the seal on your menstrual cup before removing it. Otherwise, you’re putting a lot of pressure on your vaginal canal, which your vag does not appreciate).
With Flex Cup, breaking the seal is super easy. Just pull down on the patented pull-tab. The pull-tab draws the outer lip of the cup inward, breaking the seal and keeping menstrual fluid contained. The pull-tab is also adjustable in length—perfect for those with high or low cervixes, smaller hands, or those who prefer a less messy removal.

With other brands of menstrual cups, pinch the base of the cup to break the seal before removal. Refer back to your particular brand of cup’s user guide for more information on removal.
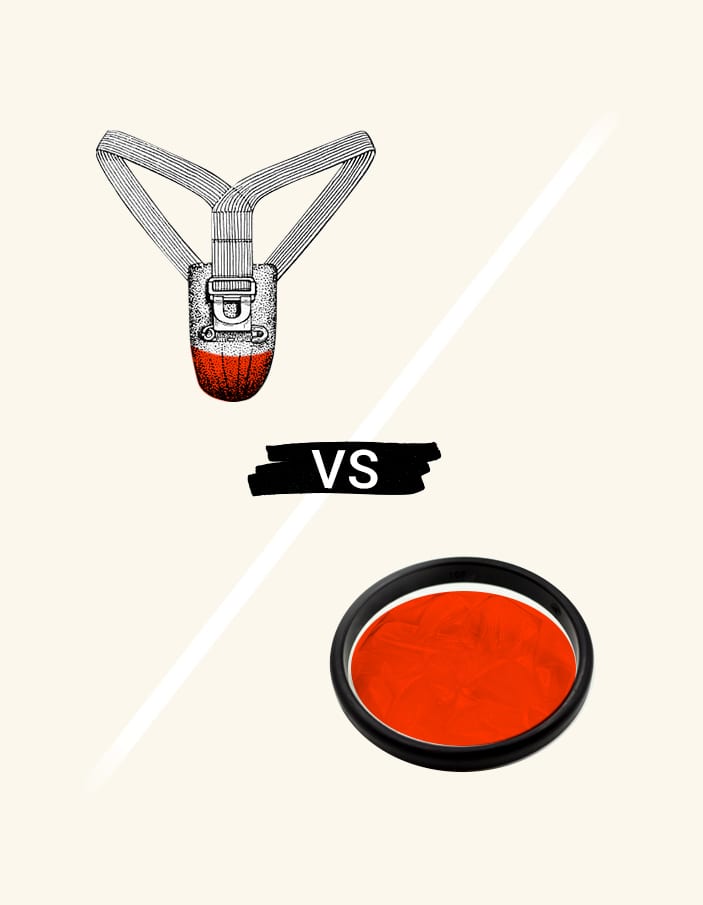
Can I use a menstrual disc with an IUD?
We’ve covered menstrual cups with IUDs. But what about menstrual discs, like Flex Disc™? For more information, we spoke with Dr. Jane van Dis, a board-certified OB-GYN with 13 years of experience. The verdict? “Flex Disc is very safe for IUD users,” she explains.
“Theoretically, I think some women are worried that, as they are removing Flex®, they might accidentally dislodge the strings of the IUD and accidentally pull out the IUD. I haven’t ever heard of a client actually being able to dislodge their IUD while they’re using a Flex Disc, but potentially that could be a concern – however, in summary, Flex is safe when used as directed, and if you have questions, contact your provider.”

Similar to our recommendation for using menstrual cups with an IUD: If you want to use menstrual discs for their many benefits including 12-hour comfort, talk to your provider. While menstrual discs like Flex Disc and Flex Reusable Disc are designed to be suction-free, your provider can confirm how your device will work with a disc based on your device’s placement, length of the strings, and position in relation to your unique anatomy.
Other FAQs: Menstrual cup & disc with IUDs
1. How soon after my IUD is placed can I use a menstrual cup or disc?
Most physicians recommend waiting at least two cycles after IUD placement before using menstrual discs or a menstrual cup. That’s because intrauterine devices are slightly more likely to be displaced during the first six weeks after insertion.4
A few months after your IUD is inserted, you’ll typically return for a follow-up appointment. This appointment is to confirm that your device is in the right place. The easiest way to do this is via a pelvic ultrasound, but your provider will also likely do a physical exam. This is a good time to discuss any concerns you may have about menstrual product use.
2. Should I get my IUD strings trimmed first?
Some individuals prefer to have their IUD strings trimmed (by their provider) so that they are flush with the cervix. This may reduce the risk of accidental IUD displacement or expulsion when removing a menstrual cup or disc. However, trimming the strings may also result in a slightly more challenging when the IUD is removed.5
You don’t have to have your IUD strings trimmed in order to use a menstrual cup or disc – just be mindful to feel for the strings when removing your menstrual product (try running a clean finger all the way around the edge of the cup or disc) to make sure they are out of the way.
3. What if I have a low cervix?
It may come as a surprise, but the cervix is not always located in the same spot. It actually moves and shifts positions throughout your menstrual cycle (and after penetrative sex, too). Some individuals, however, are born with a “low cervix.” This is normal, it just means your cervix position is a little closer to the entrance of your vaginal canal.
Typically, a cup sits in the vaginal canal, away from the cervix. If you have a low cervix, your menstrual cup may sit closer to your cervix than it would in others. This doesn’t mean you can’t use a cup with an IUD. Just be extra careful during insertion and removal, checking that your IUD strings are out of the way.
IUD users with a low cervix can also use menstrual discs, and it may make them easier to insert and remove. Menstrual discs are placed in the vaginal fornix and dont need suction to stay in place. Always make sure your disc stays tucked behind your pubic bone during use, and be gentle when pulling it out.
Disclaimer: The content of this blog post is based on information and research currently available as of the time of publication. As new information becomes available, we’ll update our content accordingly. However, if you have any specific questions Flex Cups or Discs, email us at help@flexfits.com. We also recommend speaking to your healthcare provider for additional clarity.
This article is for information only. It is not offered as medical advice, nor does it substitute for a consultation with your physician. Please consult your physician If you have any gynecological/medical concerns or conditions.
© 2023 The Flex Company. All Rights Reserved.