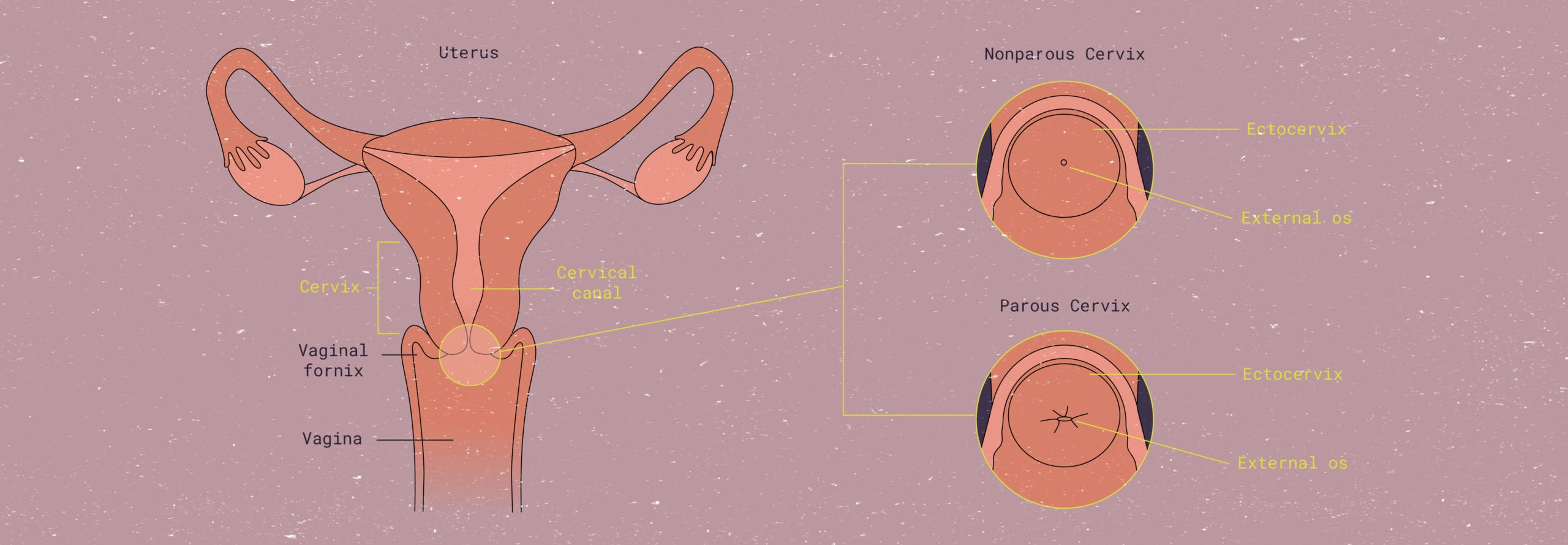
Diagram of the cervix in parous (have given birth) and non-parous (have not given birth) individuals.
The cervix: An owner’s manual
Your ultimate guide to the cervix
TL/DR: January is Cervical Health Awareness Month, and to celebrate, we’re giving the cervix center stage. This guide includes a briefer, a how-to guide on finding your very own cervix, and important info on cervical cancer prevention.
Along with popping bubbly and setting your intentions this New Year, take a moment to celebrate the one who’s been with you since the start of this wild ride… your cervix. Yeah, maybe not what you expected us to say, but a fascinating and incredible body part nonetheless.
January is National Cervical Health Awareness Month, a dedicated excuse to learn, discuss, and ask questions about the cervix. So, whether you’re an expert or you’re a total newbie to cervical health and terminology, this article is a great place to start. Read on to learn more about the little C that could.
Cervix 101: What it is & where is the cervix located
This guide will give you the down-low on your down low: We’ll tell you exactly what the cervix is and does, walk you through the steps to find and feel your own cervical anatomy, and explain how it is related to your cycle. We’ll also answer some frequently asked questions about specific parts of your cervix, its anatomy, Pap smears, HPV, and cervical cancer. Pull up a chair and let’s get to celebrating.
What is the cervix?
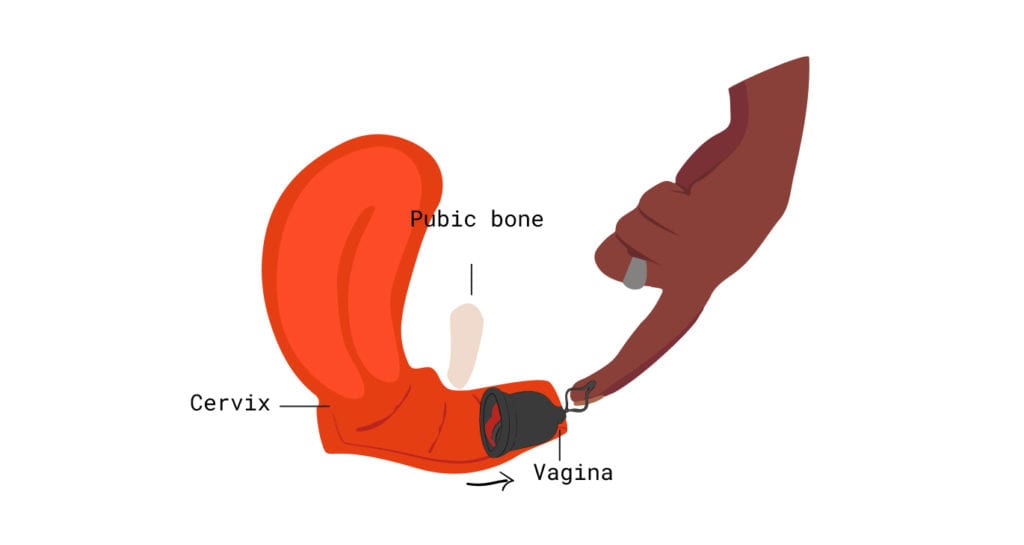
The cervix (or cervix uteri) is a canal, part of the female reproductive system. The cervix is located at the lower end of the uterus, connecting the uterus to the top of the vagina. This small but mighty organ plays a crucial role in women’s health and reproduction.
This structure divides the lower part of the uterus, known as the uterine body (a.k.a. uterine cavity), from the vaginal canal.1 It is a roughly donut-shaped structure that can contract and expand depending on what stage of the menstrual cycle you’re in, as well as throughout pregnancy.
It is basically the gateway to the female reproductive system: It lets a newborn baby out into the world, it’s the door through which your period blood flows, and it’s where an IUD must pass through during placement. When an object (or sperm) needs to get into your uterus from the outside, it must first pass through a part of the cervix called the ectocervix (by way of the external os) and then into the endocervical canal (through the internal os) before it reaches the rest of the womb or any other parts of the reproductive system.
The point where the endocervix and ectocervix meet is known as the squamocolumnar junction, also referred to as the transformation zone. The majority of abnormal cell changes and cervical cancers originate in the squamous cells of the squamocolumnar junction.
The cervix blocks bacteria and pathogens from entering your uterus, protecting you and a potential fetus. It also allows sperm to fertilize eggs, leading to pregnancy.
The average cervical canal is approximately 30 mm long.2 During labor, the mucus plug will come out and the cervix will dilate from 1cm, to 4cm in the first stage of labour, and up to 10 cm in diameter during the second stage, to let the baby pass through the birth canal. That’s more than 30 times its original size!3
For some context, 1 cm is about the size of a Cheerio, whereas 10 cm is the size of a bagel. Name any other part of your body that can expand and contract as much as the female reproductive tract in just a matter of hours. We’ll wait.
How to find & feel your cervix
Self-exploration serves as an important educational tool when it comes to reproductive health. Have you ever felt your cervix? If your answer is “no” or, “um… I don’t know?” then fear not – this next part is for you.
First, a quick reminder (and this applies to menstrual product insertion, educational exploration, and/or recreational activities down there…): Wash your hands!
It might sound obvious (especially this year, of all years), but hand-washing with hot water and soap, including under your fingernails, for more than 30 seconds is the most effective way to make sure you’re hygienic and not bringing anything into that space. Think of it as an excuse to hum the chorus of the latest Ariana Grande song.
One more thing: it’s often recommended that your nails are short or neatly trimmed to prevent any micro-abrasions, as your cervical tissue is somewhat sensitive.
- Step 1: Position: Position yourself to access the vaginal opening securely. You can stand with one leg up for leverage, ensuring you’re on a stable surface. Avoid slippery surfaces for safety. Other positions that might work: Squatting, lying on your back with knees open, or your favorite space-creating yoga position.
If you have a preferred position for inserting a menstrual cup or disc, give it a try. If you happen to have a speculum and body-safe lubricant, try inserting it while lying down and follow the next steps.
Talk to your provider for guidance on using a speculum at home for the first time. - Step 2: Timing: After a warm shower or bath, some find it easier to locate their cervix due to relaxation and warmth. Trying this outside of your period may be preferable, as period blood can make things slippery.
- Step 3: Exploration: Insert your longest finger into the vagina slowly until the first or second knuckle. Pause to locate your cervix. Depending on timing and anatomy, it may be higher or lower than expected.
In addition, keep in mind that your cervix may not be centered at the end of the vaginal canal; its “symmetry” relative to your vagina also has to do with your cycle.
Pro tip: To make things a little easier, you can lube up your finger with a tiny bit of water-based, body-safe lubricant, first.
How will you know when you’ve found your cervix?At the end of your vaginal canal, you should feel a roughly circular-shaped protrusion – this is it! Again, depending on the time of the month (more on that later), it may feel soft and squishy or firm and uniform. You may even be able to feel the cervical os, which is the tiny hole-like opening of the cervix, but don’t sweat it if you can’t.
Remember: everyone is unique! If these descriptors don’t match your cervical-finding experience, don’t worry – you’re not an alien and you’re not missing a body part. It might just take a little time to get familiar with your own internal anatomy.
To enhance the learning experience, practice feeling for your cervix at different stages of your menstrual cycle, like during ovulation (roughly halfway through your cycle) or menstruation, to see how the texture, rigidity, shape, or height of your cervix changes over time.
Want to take a photograph of your own, beautiful cervix? Pick up a self-exam kit from The Beautiful Cervix Project, a collective that encourages people with cervices to learn cervical self-exam and fertility awareness in order to promote respect, confidence, and health.
Check out more photographs of cervices submitted to the Project here. Note: External genitalia is not visible in any of the photos, but they are all taken by using a speculum to open the vagina to view the cervix. Please view at your discretion.


How deep is the cervix?
The “average” cervix is located somewhere between 2.5 and 5 inches deep within the vaginal canal. However, the look, feel, and placement (or depth) of your cervix will change throughout your cycle depending on what else is going on in your reproductive system.4 5
Also, keep in mind that these measurements can change dramatically during sexual arousal: Sexual excitement actually causes the upper two-thirds of the vagina to lengthen by forcing both the cervix and uterus to ascend (i.e. move higher up within your body).
How the cervix changes position throughout your cycle
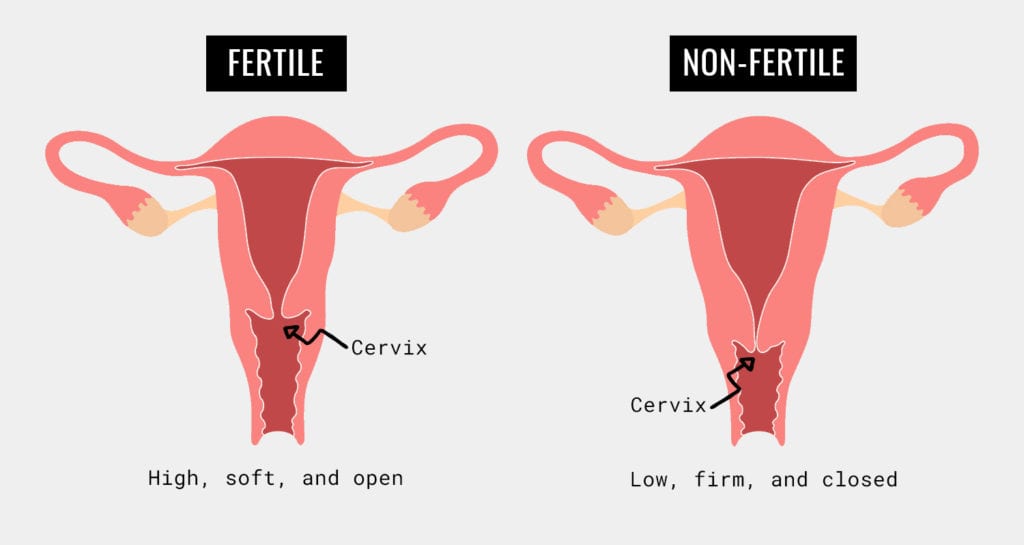
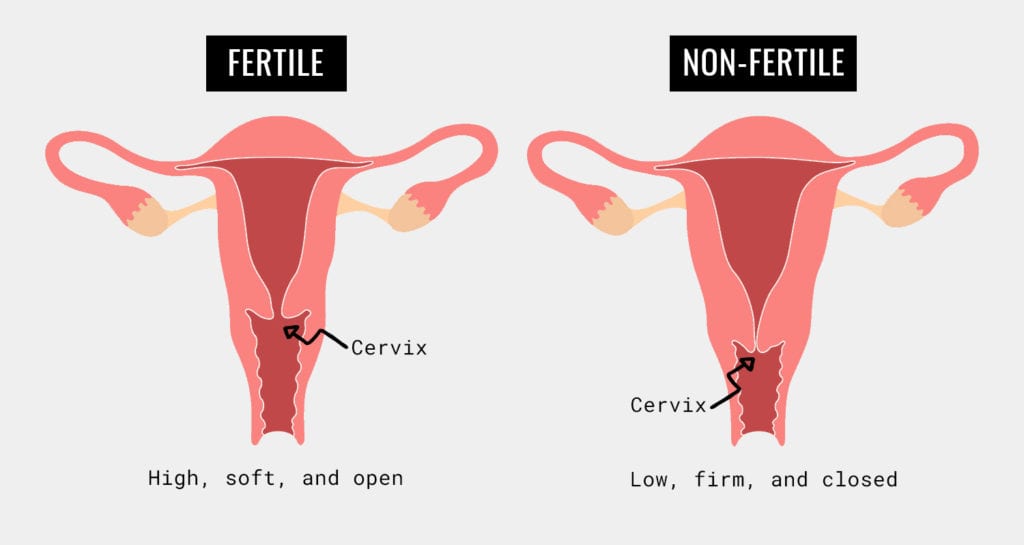
During ovulation, the cervix is wholly focused on allowing sperm to enter the body of the uterus so they can swim upwards and join with the released eggs for fertilization. Here’s a helpful acronym to remember what it is like during ovulation: SHOW. Soft, high, open, and wet.
The cervix will be softer, almost comparable to the softness of your lips; it will be high, i.e. located deeper in the vaginal canal; it will be open, so that the cervical os can allow sperm to enter; and it will be wet, meaning that it is releasing protective secretions to protect the local environment from the relatively acidic sperm.
As you approach menstruation, the cervix will feel firm and harder to the touch, something like the cartilage of your ear or the tip of your nose, and will also drop lower. The cervical os will become smaller, and generally produces less discharge during this time (in your luteal phase) when compared to ovulation.
Another really interesting fact about the cervix? Not only does it change its position or “height,” but it may also change its angle in relation to the vaginal canal. This means that, if you imagine the cervix as a donut, the hole of the donut may rotate to point upwards, downwards, or even out to the side.
Like most cervical changes, this is subject to individual variation and may also depend on the shape of your uterus. For example, if you’ve been told by a healthcare provider that you have a retroverted uterus, then your cervix may be angled upwards at its “baseline.” FYI, an estimated 20% of the population has a retroverted uterus.6
To summarize, the cervix moves and changes texture throughout your cycle. During ovulation the cervix will SHOW (soft, high, open, wet) us it’s ready for fertilization, whereas during menstruation it will be harder to the touch and lower, with less discharge (no acronym for this one – but let us know if you think of one!).
Using menstrual cups & discs with a high or low cervix
Remember that when the lining of the uterus sloughs off, the menstrual blood exits through the cervical os, so, when choosing a menstrual product, it may be helpful to think about your unique cervical position. The cervix changes throughout the cycle, but each person has unique variations in its baseline position and texture, including height in the vaginal canal and os angle.
Individual differences can affect the comfort and effectiveness of menstrual products like cups and discs placed near the cervix. With a low cervix, it may be challenging to position a menstrual cup due to limited space in the vaginal canal.
Think back to that magical moment when you felt your cervix for the first time. It may have taken a couple tries, and some very experimental stretching, but you felt something that maybe, possibly is your cervix.
Do you remember how many knuckles of your finger were inserted at that time? How about this: did you have to angle deeper, or did you feel it fairly soon upon insertion? These are clues that can let you know whether you might have a low, high, or average cervix at baseline.
If you think you may have a low or high cervix and you’ve been having a hard time with certain period products (i.e. leaks, discomfort), here are a few tips from the Flexperts:
LOW CERVIX & PERIOD PRODUCTS:
A low cervix will sit closer to the vaginal opening within the canal. It may require only one to two knuckles to feel, as opposed to the entire finger.
If your cervix sits low, it may be a bit easier to insert and remove products like Flex Disc™ since you won’t have to reach as far into the canal. However, make sure that you continue to push the rim of the disc down (towards your tailbone) such that it completely surrounds cervical os – and then tuck the front rim behind your pubic bone.


If you struggle to use a menstrual cup with a low cervix, it might be because the cup is too long for your vaginal canal depth. This can lead to the rim not creating a complete seal beneath the cervix.
A low cervix may sit inside your menstrual cup. If you suspect this issue, run your finger around the cup’s rim to locate the cervix. Pinch the base of the cup and pull it down below the cervix. Angle the cup towards your cervix and do a finger check for proper positioning.
If you have a low cervix, consider emptying your menstrual cup more frequently or opting for a larger size to prevent menstrual cup leakage caused by your cervix taking up space in the cup.
HIGH CERVIX & PERIOD PRODUCTS:
A high cervix sits deeper within the canal, requiring the full length of a finger to reach. All period products can be used, but you may need to experiment with insertion and removal techniques until you find what works best for you.
Menstrual disc removal may be a challenge for folks with a high cervix – and cup removal, too, especially if the cup you use doesn’t have a pull-tab to grasp.
For easier disc removal, if your cervix is high, bear down on your pelvic floor muscles as if trying to poop. This should help move the disc downwards for easier removal.
When using a menstrual disc, those with a high cervix may not push it in far enough initially, leading to leakage or discomfort. Angle the disc downwards and push it back into the posterior fornix, securing the front rim behind your tailbone.
Are you a menstrual cup user with a high cervix? You may prefer a longer cup or one with a pull-tab (like Flex Cup™) so that it’s easier to grasp for removal. Remember, you want your menstrual cup to sit close enough to the cervical opening to create a complete seal, collecting your period blood leak-free.
If you feel like you have to shove your cup so far up that it’s almost out of reach – and super annoying to remove – take a longer or larger capacity cup for a spin.
“AVERAGE” CERVIX & PERIOD PRODUCTS:
An average cervix is… trick question, there’s no such thing! The position of the cervix is relative to the person it’s in. What is high for you may be average for another, and vice versa. This goes to show why self-exploration is an important tool for understanding your body.
Not all period products suit every body type. If you’ve been struggling with a product for months and still experiencing leaks or discomfort, it may be time to switch.
Even switching brands can help: Some users that haven’t been able to get Flex Disc to work, for instance, have found success with our other menstrual disc brand, Softdisc. Softdisc looks and feels similar to Flex Disc, but its rim is made of a different polymer that works better for some folks.
For detailed guides on how to insert Flex Cup and Disc, click here.
Cervix 201: Pap smears, cervical cancer research, nabothian cysts HPV & Pregnancy
On a more serious note, cervical health awareness includes being aware of cervical cancer. Cervical cancer used to be one of the leading causes of death for women in the United States; however, in recent years, this number has gone down – largely as a result of increased Pap smears as well as the HPV vaccine (see: HPV Testing, below, for more information on this).7
Even with improving numbers, we must remain vigilant. In 2017, the CDC reported over 12,000 new cases of diagnosed cervical cancer in the US, causing over 4,000 deaths.8 HPV is the leading cause, a virus transmitted through sexual contact.7 Awareness is key to maintaining cervical and overall health.
Pap smears
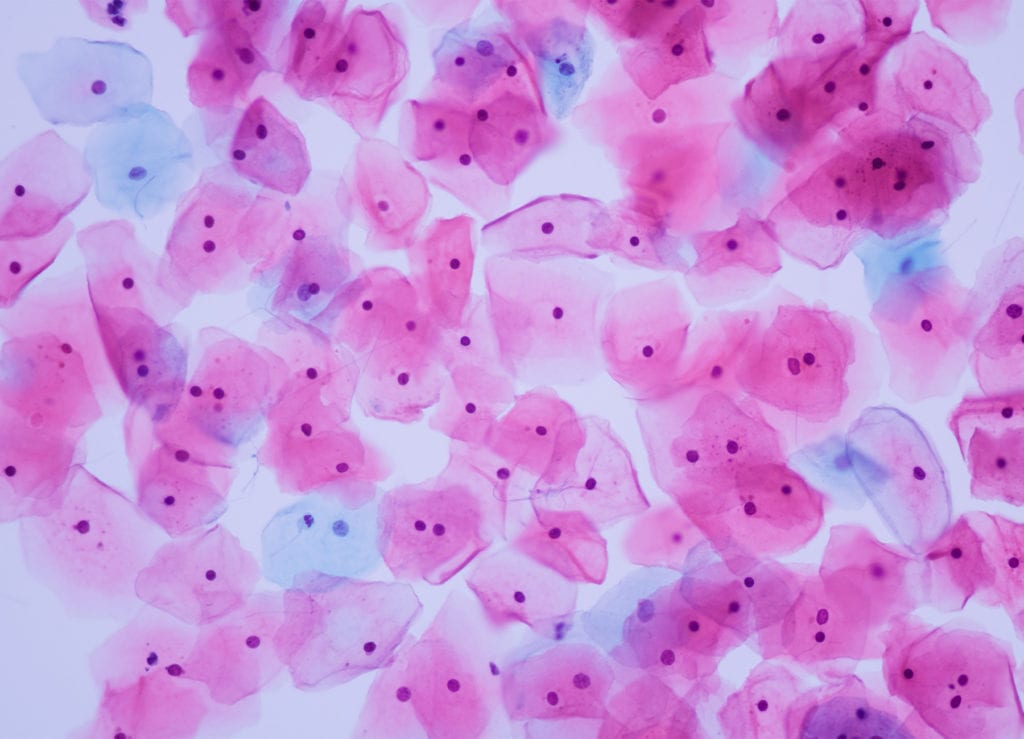
The most common screening tool for cervical cancer is the Pap smear. If you have not had one, here’s what to expect:
The healthcare provider will use a lubricated speculum to inspect the cervix by opening up the vaginal walls.
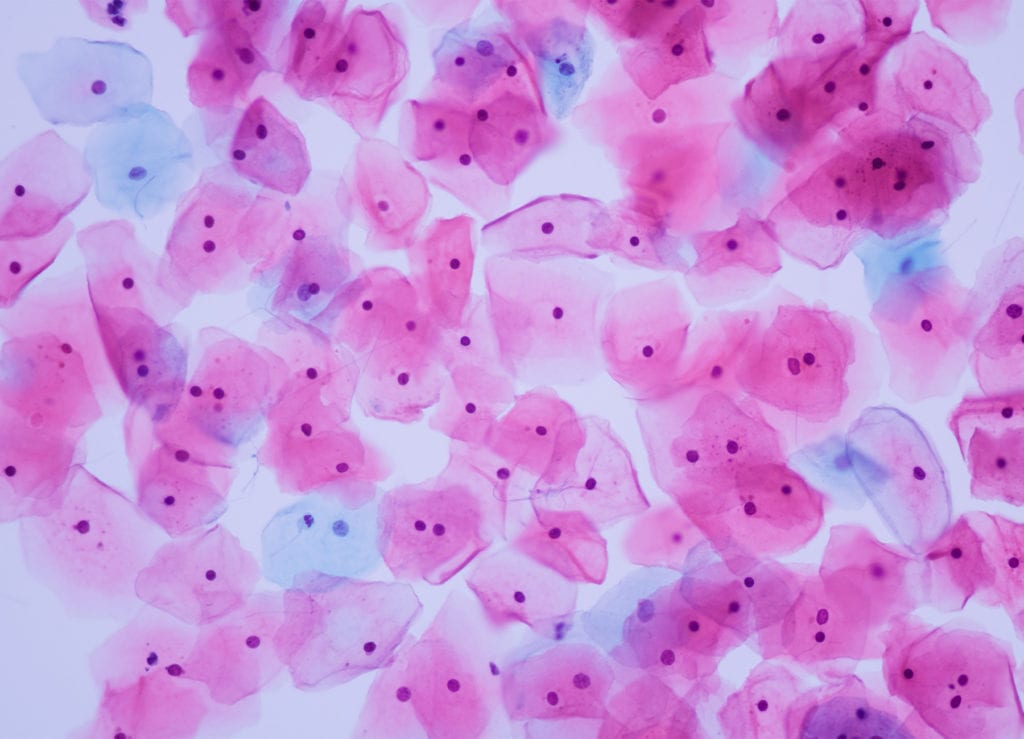
Your provider will visually examine the area and using a spatula, brush, or cytobrush, will take a small tissue sample of the surface of the cervix for testing.
They lightly scrape cervical tissue to test for abnormalities. Results are expected quickly due to the routine nature of the procedure.
Does a Pap smear hurt?
It may not be 100% comfortable, but for most, it’s like a quick scratch – not unbearable and over quickly (faster than a flu shot!). If you’re anxious, talk to your provider. They’ll guide you through the process and calm your nerves.
Can you get a Pap smear during your period?
According to the American Society of Clinical Oncology, “the best time to schedule your Pap test is at least 5 days after the end of your menstrual period. A Pap test can be done during your menstrual period, but it is better to schedule the test at another time.”
Yes, you can technically get your Pap done during your period. However, talk to your provider if your appointment coincides with your period as they may prefer to reschedule.
How often should you get a Pap smear?
The guidelines for cervical cancer screening may vary annually. Most professional societies (ACOG, USPSTF) recommend individuals AFABAFAB stands for “assigned female at birth.” have a regular pap smears every 3 years from age 21.9 Frequency may be adjusted after age 30 and menopause based on health history and prior screening results.
HPV Testing: When is it necessary?
HPV, short for human papillomavirus, is a group of viruses transmitted through sexual contact. There are over 100 types, classified from low to high risk in terms of prognosis. Most are low-risk.
Some HPV strains are asymptomatic, while others can cause genital warts or warts around the anus, mouth, or throat. Certain high-risk types of HPV can lead to cervical and other cancers.
Most healthcare providers offer HPV testing along with a Pap smear, as both can be done on the same cell sample, known as “co-testing.”
Many professional societies state that the co-test is a good way to minimize the frequency of screening. For example, instead of coming in to do a Pap smear every 3 years, you might be able to come in once every 5 years and have both a Pap smear and HPV screening test done at the same time.
Another note on HPV: There is currently a vaccine available for HPV prevention, called Gardasil 9, and it is more than 99% effective.10 The target group for this vaccination is all genders at 11-12 years of age — but it can also be given safely to older teens and adults. It’s a two-part vaccine, with a second dose that must be administered within 6 to 12 months of the first.
Learn more about the HPV vaccine on the CDC website.
If you have any other questions about Pap smears, co-testing with HPV tests, and/or the HPV vaccine itself, have a conversation with your healthcare provider or OB-GYN.
Nabothian cysts vs. cervical cancer
Nabothian cysts (or nabothian follicles) are benign lumps that may develop when glands in the cervix become blocked with skin cells. If discovered during a pelvic examination, there is no need for concern as they are prevalent and typically do not need treatment.
A nabothian cyst is a cyst filled with mucus located on the cervix’s surface. It typically occurs when the stratified squamous epithelium of the ectocervix covers the simple columnar epithelium of the endocervix, leading to blockage of the cervical crypts and the accumulation of cervical mucus within them.
Nabothian cysts sometimes form after you’ve had chronic inflammation in your cervix (such as an infection of the cervix or chronic cervicitis).
Cervix anatomy changes and pregnancy
There’s no doubt that the uterine cervix plays a crucial role during pregnancy. This is why, as soon as your pregnancy test comes positive and is confirmed, your healthcare provider will begin regular cervical checks. Here’s a couple things they will be monitoring.
Cervical length
Cervical length is the measurement of the lower end of your uterus, and it’s different from cervical depth. Healthcare professionals monitor this during pregnancy for signs of premature labor. If you experience short cervical length too early in pregnancy or if it is slightly open, your baby may be at higher risk for premature birth and the Doctor might recommend a treatment like vaginal progesterone to prevent preterm labour. Deliveries between 20 weeks of pregnancy and 36 weeks and 6 days are considered preterm.
Cervical insufficiency
Sometimes, the cervix can become thin and open too soon during pregnancy, typically without any pain or contractions. This is known as cervical insufficiency or incompetent cervix. It can contribute to premature births or pregnancy loss.
Cervical insufficiency cannot be diagnosed before pregnancy. It’s crucial to inform your healthcare provider of any symptoms. Although there typically no prior indication of cervical insufficiency, some may exhibit symptoms like vaginal pressure, spotting or vaginal bleeding, abdominal or lower back pain, or vaginal discharge. Treatments may involve progesterone supplementation, periodic pelvic exams, and cervical cerclages.
Fun facts about your cervix
To wrap up this guide, here are a couple of fun facts. Now you’re totally armed and ready for your next trivia night (you’re welcome).
1. It is flexible. It expands up to 10 cm during pregnancy and childbirth, only to return to its original size after delivery. Talk about resilience.
2. It can bruise during intercourse from excessive pressure. Rest usually resolves it in a few days, but if pain persists, consult your healthcare provider.
3. There’s a thing called a cervical orgasm, which is not about cervical penetration as some believe (which is impossible). It’s a powerful orgasm from deep penetrative sex with the right cervical pressure and surrounding tissue, thanks to cervical nerve pathways related to sexual response.11
4. It produces mucus. Also known as vaginal discharge, your cervix has glands that produce a clear, viscous, alkaline mucus. The consistency and texture of your cervical mucus changes throughout your menstrual cycle, as well as during pregnancy. Depending on where you are on your cycle you can experience thin or thick mucus, color can also change.
5. It is unique, playing a similar role in structure and function for everyone. Each one is beautiful and as unique as the individual it belongs to. Let’s show some love to our friend, the cervix, this Cervical Health Awareness Month.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2025 The Flex Company. All Rights Reserved.
- Anatomy of the Female Pelvis. SEER Training Modules, Cervical and Uterine Cancer. U. S. National Institutes of Health, National Cancer Institute. Retrieved December 30, 2020, from https://training.seer.cancer.gov.[↩]
- Salomon, L. J., Diaz-Garcia, C., Bernard, J. P., & Ville, Y. (2009). Reference range for cervical length throughout pregnancy: non-parametric LMS-based model applied to a large sample. Ultrasound in Obstetrics & Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology, 33(4), 459–464. https://doi.org/10.1002/uog.6332[↩]
- Hutchison, J., Mahdy, H., & Hutchison, J. (2020). Stages of Labor. In StatPearls. StatPearls Publishing. PMID: 31335010.[↩]
- Casey, P. M., Long, M. E., & Marnach, M. L. (2011). Abnormal cervical appearance: what to do, when to worry?. Mayo Clinic Proceedings, 86(2), 147–151. https://doi.org/10.4065/mcp.2010.0512[↩]
- Planned Parenthood. What is the Cervical Mucus Method?: Cycle, Stages & Chart. Retrieved December 30, 2020, from https://www.plannedparenthood.org/learn/birth-control/fertility-awareness/whats-cervical-mucus-method-fams[↩]
- Haylen B. T. (2006). The retroverted uterus: ignored to date but core to prolapse. International urogynecology journal and pelvic floor dysfunction, 17(6), 555–558. https://doi.org/10.1007/s00192-005-0051-0[↩]
- CDC. (2020, August 31). Cervical Cancer. Retrieved December 30, 2020, from https://www.cdc.gov/cancer/cervical/index.htm[↩][↩]
- U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2019 submission data (1999-2017): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; www.cdc.gov/cancer/dataviz, released in June 2020.[↩]
- ACOGACOG stands for the American College of Obstetricians and Gynecologists (a professional membership organization for obstetrician–gynecologists).. (2018, April). Cervical Cancer Screening. Retrieved December 30, 2020, from https://www.acog.org/womens-health/faqs/cervical-cancer-screening[↩]
- ACOGACOG stands for the American College of Obstetricians and Gynecologists (a professional membership organization for obstetrician–gynecologists).. (2017, June). Human Papillomavirus Vaccination. Retrieved December 30, 2020, from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2020/08/human-papillomavirus-vaccination[↩]
- Komisaruk, B. R., Beyer-Flores, C., & Whipple, B. (2006). The science of orgasm. JHU Press.[↩]