Tilted, slanted or tipped: What is a retroverted uterus?
A tilted uterus is more common than you might have thought
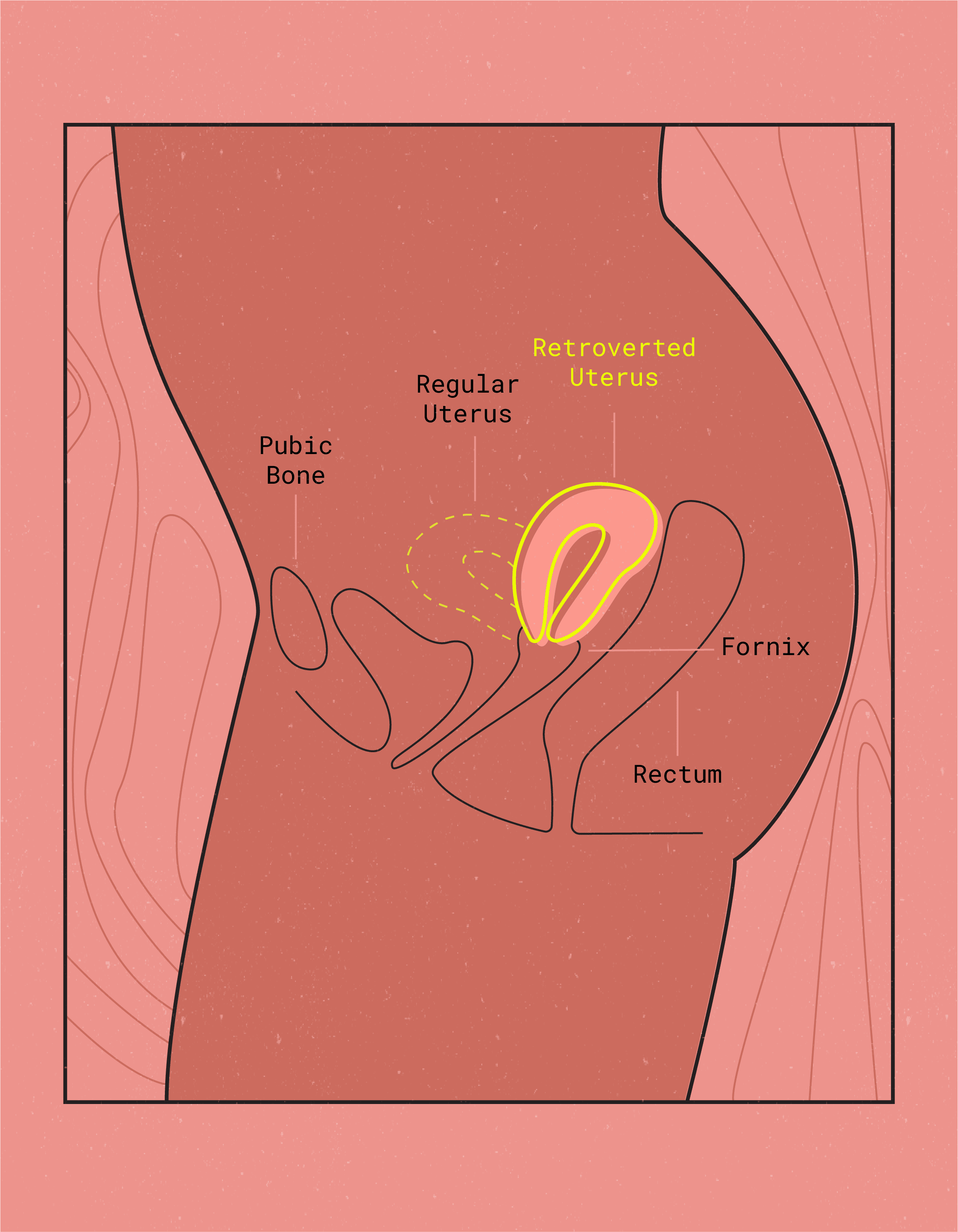
TL/DR: One in five people with vaginas have what’s known as a tilted, or retroverted, uterus. Instead of pointing forward toward the belly button, a retroverted uterus points in the opposite direction, towards the lower back.
All kinds of images come to mind when you hear the words ‘tilted,’ ‘slanted,’ or ‘tipped’. A spilled drink, perhaps a bookshelf that was installed incorrectly, or maybe an off-center picture frame? No big deal, right? When used to describe the uterus, however, those three words can lead to panic.
Well, we’re here to tell you not to panic. A tilted, AKA retroverted uterus (or matrix) is a common anatomical anomaly (how’s that for a tongue twister?). It is seen in approximately one in five individuals assigned female at birth.1
Typically, the uterine cavity points forward toward the navel. When it is tilted or retroverted, it points backwards and down towards the lower back, instead. Additionally, from being in a retroverted position (pointing backwards), some uterus-havers can experience a retroflexed uterus when it is also bent backwards.

A tilted or retroverted uterus may not always cause symptoms. If symptoms do occur, they can often be managed with lifestyle changes.
Here’s the lowdown on retroverted uteruses:
What are the signs & symptoms of a retroverted uterus?
Only some individuals with a tipped matrix or with uterine retroflexion experience symptoms. They may include:
- Vaginal, lower back or pelvic pain during sexual intercourse,
- Painful periods, a.k.a. dysmenorrhea,
- Slight urinary incontinence, and
- Feeling of pressure on the bladder.2
If you notice any of these signs or symptoms, consult your doctor or OB-GYN. A retroverted uterus diagnosis is not a cause for concern. Your doctor will provide treatment options and recommendations to manage any discomfort. In extreme cases, medical professionals might recommend a uterine repositioning surgery.
However, it’s important to rule out other potential causes for painful periods, urinary issues, or pain during sex.

What are the causes of a retroverted uterus?
Some individuals are born with a tilted matrix – in these cases, it’s just a roll of the genetic dice. Others may experience uterine retroversion after menopause or following childbirth, due to loosening of the ligaments that hold the uterine cavity upright.
In some cases, uterine scar tissue from conditions or procedures can pull the uterine cavity backward, leading to retroversion. These could include endometriosis, pelvic surgeries and uterine fibroids. Tumors, adhesions, and/or infections of the uterus or fallopian tubes such as pelvic inflammatory disease (PID) are also included.3
Retroverted Uterus Pregnancy: What you need to know
Pregnancy can also cause uterine retroversion, with the position of the uterus changing intermittently during gestation. A tilted matrix occurs in 10-20% of pregnancies in the first trimester.4
A tilted uterus during pregnancy is typically temporary and rarely causes complications. One of these extremely rare conditions is called incarcerated uterus. Uterine incarceration occurs when the pregnant retroverted or retroflexed uterus grows and becomes wedged into the pelvis.
How is retroversion diagnosed and what tests are needed?
Routine pelvic exams are a great starting point to discard many issues your vagina might have. However, your doctor or OB-GYN will request a transvaginal ultrasound or MRI in order to diagnose a retroverted or tilted matrix.5
During the ultrasound, your doctor or a technician will insert a wand into your vaginal canal. In order to obtain a clear view of the exact position where your uterine cavity sits, your bladder needs to be emptied before the procedure. The ultrasound only takes a couple of minutes and you’ll likely find out the results right away.

Sex, pregnancy & fertility with a retroverted uterus
In the past, doctors believed that a tilted matrix could cause fertility problems. However, research has shown that sperm can navigate various uterine shapes and sizes. Recent studies have shown that a tilted or retroverted matrix doesn’t have any impact on a woman’s fertility.6
Rarely, scar tissue in the uterine cavity can cause a tilt and make it harder for sperm to reach an egg. It can be caused by endometriosis, infections, or prior surgeries.6 If you’re worried about conceiving, consult your OB-GYN or fertility specialist.
In terms of your sex life, a tilted uterus may not create any problems whatsoever. For those who do notice pain or discomfort during intercourse, experiment with new positions until you find what works for you.
Why do some people with tilted uteruses deal with painful intercourse while others don’t?
It’s because every tilt is different. A tipped uterine cavity can affect the angle at which the vagina meets the cervix and the orientation of the pelvic floor muscles.7
For some, positions in which the pelvic muscles are getting a ton of repeated pressure don’t feel so great.
Tip: People with a retroverted uterus often find face-to-face positions most comfortable for penetrative sex. Another option is a “cross-wise” position.78
How a retroverted uterus could impact your period
Want to find out how a tilted uterus could affect your period? Dr. Jane van Dis, a board certified OB-GYN with 13 years of experience tells us all about it.
“Individuals who have a retroverted uterus often complain of more painful periods,” she explains. “Some might find Flex Disc™ more comfortable [than other menstrual products] because the Disc sits at the top of the vagina — the widest portion of the vagina — thus limiting the amount of pressure on vaginal walls.” Since the orientation of your pelvic floor muscles might differ with a retroverted matrix, less vaginal pressure usually = less discomfort.
It’s true: Dysmenorrhea (intense period pain) is more common in those with a tilted matrix.3 It’s thought that the body has to cramp a little bit harder to push out menstrual blood. The angle of retroversion may explain to some extent, how much pain is experienced.
A study found that increased period pain intensity was associated with more extreme angles of uterine flexion, regardless of its direction (forward or backward).9
If you’re experiencing severely painful periods, don’t immediately jump to conclusions and assume you have a retroverted matrix. Dysmenorrhea has many possible causes: Talk to your doctor or OB-GYN to rule out other conditions.

Can a retroverted uterus be corrected and how?
A retroverted uterus, where the uterine cavity tilts backward instead of forward, can often correct itself naturally over time. However, if it causes discomfort, a doctor may recommend exercises to strengthen the pelvic muscles or surgical intervention to reposition the uterine cavity.
Retroverted Uterus: Key Takeaways
One in five people have a tilted uterus: It’s totally common and isn’t considered a medical problem but a normal anatomical variation. While some people don’t feel any symptoms, others experience more painful periods, bladder pressure or discomfort, and/or painful sex. For some, a retroverted position of the uterine cavity can also make tampons pretty uncomfortable.
If you have a retroverted uterus, consult your doctor first for symptom management. There are online groups and forums dedicated to discussing tilted uteruses that may be helpful. Talk to your partner about finding sex positions that are comfortable and pleasurable for both of you. You can also experiment with different menstrual products to manage your period.
At the end of the day, the most important thing to remember is to listen to your body. If you’re experiencing pain, don’t ignore it – seek professional advice ASAP.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2024 The Flex Company. All Rights Reserved.
- 2020, March 31). U.S. National Library of Medicine. Retrieved from https://medlineplus.gov/ency/article/001506.htm[↩]
- Whelan, C. (2019, April 9). Retroverted Uterus: Causes, Fertility, Treatment, and More. Healthline. Retrieved from healthline.com/health/womens-health/tilted-uterus[↩]
- Retroversion of the uterus. (2020, March 31). U.S. National Library of Medicine. Retrieved from https://medlineplus.gov/ency/article/001506.htm[↩][↩]
- O’Grady, J. P. (2018, August 1). Malposition of the Uterus: Overview, Uterine Retroversion or Incarceration, Uterine Torsion. Medscape. Retrieved from emedicine.medscape.com/article/272497-overview[↩]
- Haylen, B. T. (2006). The retroverted uterus: Ignored to date but core to prolapse. International Urogynecology Journal, 17(6), 555-558. doi:10.1007/s00192-005-0051-0[↩]
- Tobah, Y. B. (2019, November 22). Tilted uterus: Can it lead to infertility? Mayo Clinic. Retrieved from mayoclinic.org/tilted-uterus/expert-answers/faq-20058485[↩][↩]
- Joannides, P. (2012, May 22). A Tipped Uterus and Intercourse Positions. Psychology Today. Retrieved from psychologytoday.com/us/blog/you-it/201205/tipped-uterus-and-intercourse-positions[↩][↩]
- Pelvic relaxation and retroverted uterus. (2018, August 8). UNC Department of Obstetrics & Gynecology. Retrieved from med.unc.edu/obgyn/patient_care/specialty-services/our-services/pelvic-relaxation/[↩]
- Cagnacci, A., Grandi, G., Cannoletta, M., Xholli, A., Piacenti, I., & Volpe, A. (2013). Intensity of menstrual pain and estimated angle of uterine flexion. Acta Obstetricia et Gynecologica Scandinavica, 93(1), 58-63. doi:10.1111/aogs.12266[↩]