Briefing you on the latest in reproductive health research
TL;DR: In this month’s issue of period and health research updates, we discuss AI approaches to cervical cancer screening, updates in how cervical cancer is treated post-hysterectomy, a study that looked at long-term mental health outcomes of children whose birthing parent had high blood pressure, and some emerging data about how folks with PCOS fare with Covid-19 infections. Buckle up reader, class is in session.
AI’s next venture: The Pap smear
AI seems to be everywhere these days, from Siri telling you the best coffee shop in the neighborhood to period tracking apps that predict your cycle almost to a tee. One thing that wasn’t on our 2021 bingo cards? AI-enabled Pap smears. Yes, you heard us right.
A research team has developed a deep-learning algorithm that is able to analyze images taken from Pap smears to predict atypical cells.1
For those of us who haven’t had a Pap smear, here’s how it usually goes down: the provider uses a speculum or other such instrument to gently visualize the cervix. Then, they will reach in and, using a mini-spatula type of tool, swish around your cervix to collect cells from that area. Later, that sample usually goes into another bottle with solution in it and it’s sent to the lab for analysis.
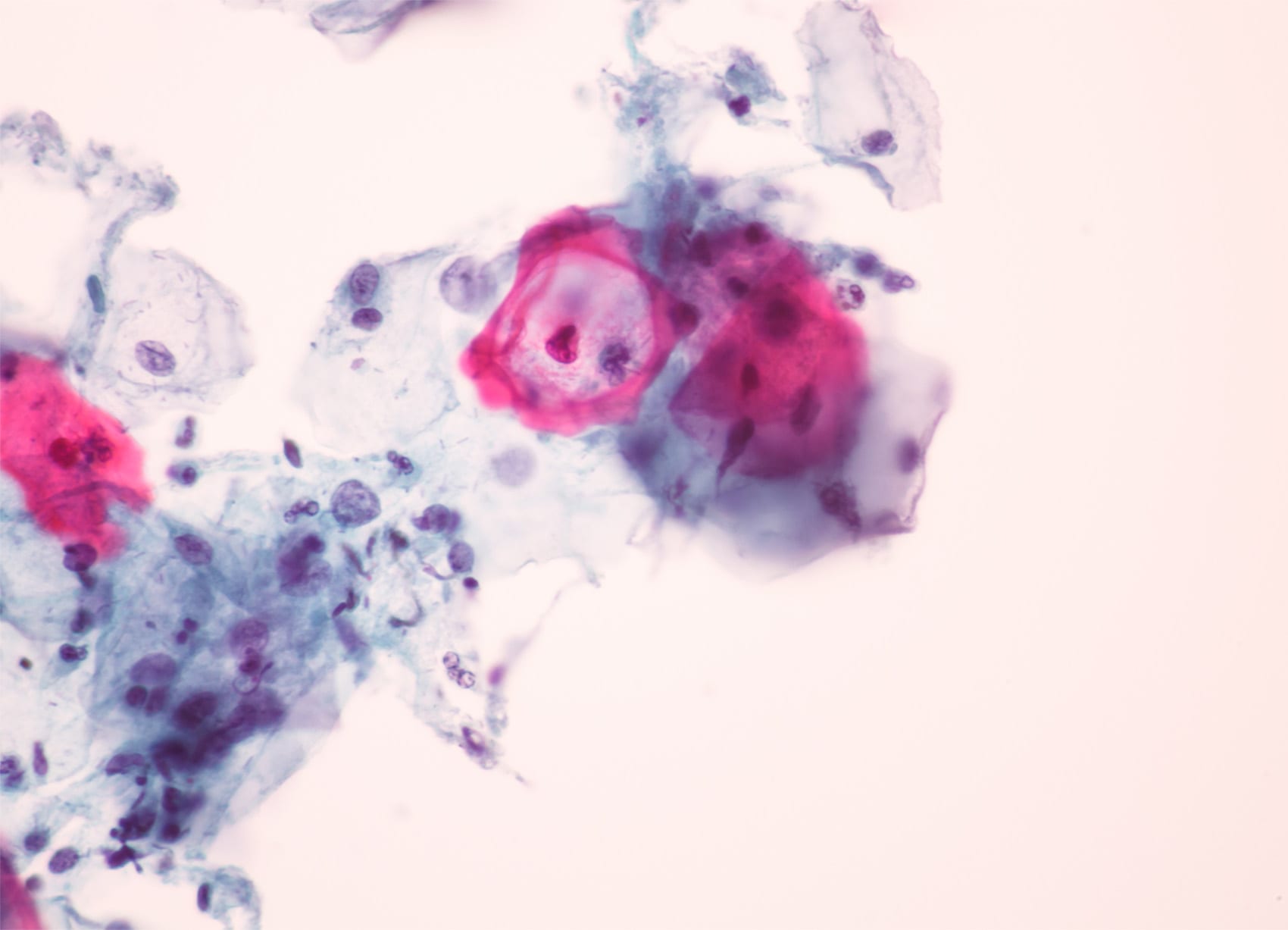
PS: Check out the photo above to see what HPV cells look like under a microscope.
The analysis process can take anywhere from days to weeks depending on the speed of the lab. Often, there’s a component of the analysis that is automatic as well as manual, meaning a highly skilled specialist in pathology or cytology will examine the sample to assess for any abnormalities.
This method of analysis is the gold standard when it is able to be done — but in places where there isn’t reliable wireless internet, or where there’s a physician shortage, it just may not be possible. People with cervixes deserve access to preventative health services like Pap smears, whoever and wherever they are.
This study provides a possible exciting solution, increasing access to cervical cancer screening for people in resource-limited areas. The study enrolled over 700 self-identified women between the ages of 18 to 64. Cervical Pap smears were collected from all women, digitized on a portable scanner, and integrated into a deep learning system that was validated by a trained pathologist.
The results from the AI model were then compared to the individually (human) analyzed results. The study found that the sensitivity for detecting atypia using AI was greater than 96%, and it was more specific for high-grade, or more progressive, lesions. Excitingly, no slides that were manually classified as high grade were incorrectly read as negative by the model – in other words, the model didn’t “miss” any concerning findings.
What does this mean going forward? The authors contend that this is an early-stage study and there are, of course, limitations. Yet these initial findings are encouraging and could provide a window to increasing access to preventative reproductive care for all.
Updates in cervical cancer treatment after hysterectomy
In other cervical cancer news, a landmark study has come out comparing results from a clinical trial treating early-stage cervical cancer after hysterectomy (the surgical removal of the uterus).2 This was a Phase 3 trial, which is one of the final stages before a treatment is up for FDA approval.
The trial included over 1000 women who were randomly assigned to receive either sequential chemoradiation, concurrent chemoradiation, or radiation therapy alone to treat their cancer. BTW, concurrent chemoradiation (CCRT) is when chemotherapy is administered on the same day as radiotherapy – whereas sequential chemoradiation (SCRT) is when treatment is administered as two to four cycles of chemo prior to radiotherapy.
The main outcome was death-free survival. In all, the SCRT produced the best results of the three modalities. This means that patients in the sequential chemo arm had a higher rate of death-free survival (or, lived longer overall), and a decreased cancer death risk (meaning, less risk of dying from their cancer).
There was no significant difference found between concurrent chemoradiation and radiation therapy alone. This result provides greater insight into the management of cervical cancer patients and a way forward to continued delivery of high-quality gynecologic cancer care.
Hypertension during pregnancy & neurodevelopmental outcomes
Moving onto updates in pregnancy research: This month, there’s new data emerging on the potential effects of hypertension during pregnancy. To recap, hypertension is the medical term for high blood pressure.
High blood pressure can cause multiple health issues, and they’re often made worse during pregnancy. A birthing person who has chronically high blood pressure during pregnancy can experience uncomfortable symptoms like headache or lower leg swelling. If it isn’t addressed, hypertension can lead to a condition called pre-eclampsia, a potentially dangerous pregnancy complication that can impact both mother and newborn.
These researchers hoped to answer the question of whether hypertensive disorders of pregnancy (HDP) are associated with neurodevelopmental outcomes in babies, independent of the confounding factor of family history.3 They used a cohort study, which is when researchers follow a group of patients over time and observe what happens, oftentimes without a specific intervention.
In this cohort, there were over a million individuals included from a Swedish registry that were followed for over two decades. They specifically looked at whether children born from mothers with hypertensive pregnancy disorders ended up developing any of the following:
- Autism spectrum disorder
- Attention-deficit hyperactivity disorder
- Intellectual disability
The researchers made sure their findings were independent of factors related to family history, with the intention to select for the number wherein maternal hypertension could be the underlying cause of the disorder.
The analysis showed that there was a slight increase in risk for developing one of these disorders later in life for those whose mothers experienced gestational hypertension. However, analyses of sibling pairings didn’t reach statistical significance.
Overall, the researchers concluded that this study is suggestive of a link, but more research needs to be done to understand this link. In general, the key takeaway here is that controlling blood pressure – and other significant health conditions – during pregnancy is super important for the long-term health of both parent and child.
PCOS and Covid-19 infection risk data emerges
One of our goals here at Flex® is to use our platform to shed light on reproductive health conditions (especially those associated with menstruation) that may not always get mainstream press – conditions like PCOS and endometriosis.
And this month, we have some new research that touches on the intersection of PCOS with that other health topic that’s been eating up your news feed for the past 12+ months: Covid-19. Specifically, researchers wanted to find out if having PCOS impacts your risk for contracting the novel coronavirus.
PCOS has been linked to insulin resistance and metabolic syndrome-type signs, which increases health risks overall – as well as impacts one’s ability to overcome infections. One research group sought to find out whether women with PCOS are at greater risk for Covid-19 compared to the general population.4
This U.K. study utilized a database of over 20,000 women with PCOS, age-matched to controls that did not have PCOS, and observed how these women fared with respect to their health over the first six months of 2020 during the early days of the pandemic. The main outcome was Covid-19 diagnosis, and other measures such as age, BMI, and concurrent cardiovascular disease were also included to provide a holistic picture of each participant’s health.
In the fully adjusted model, e.g. where variables were controlled as much as possible, the researchers found that women with PCOS had a 28% increased risk of being diagnosed with of Covid-19. The researchers concluded that people with PCOS have an increased risk of infection as found by their data.
This study is certainly stunning, but in some ways unsurprising. PCOS is often associated with metabolic syndrome, and many of these signs and symptoms (high blood sugar, central adiposity, cardiovascular disease like high blood pressure) can make it more difficult to recover from anything that is hard on the body like a serious infection.
One specific mechanism that researchers have proposed to explain the higher rate of Covid-19 infections in PCOS folks? Differential response to infection based on specific immune factors that may be modulated by, or affected by, PCOS.
One recent population study found that women with PCOS had high macrophage activation markers, but low protective markers.5 Macrophages are one of the key members of the immune system, and they are responsible for mounting an immune response; they also help to create many of the symptoms of illness that can experientially feel uncomfortable as they initiate that inflammatory response.
This study concluded that it was moreso the obesity that was associated with PCOS (as opposed to PCOS in and of itself) that could be behind the increased risk of infection. Hopefully, there’s more research on the way. Overall, it’s still exciting that more women, and women with complex menstrual conditions, are being included as the focus of research.
That’s all for this month’s round-up of period and health research updates. Tune in next month for more to come.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2021 The Flex Company. All Rights Reserved.