Ask an Ob/Gyn: Can tampons cause yeast infections?
TL/DR: While there’s no scientific proof that tampons cause yeast infections, they can disrupt the vaginal mucosa. In some cases, irritate the vaginal walls – increasing your discomfort. OB-GYN Dr. Jane van Dis drops some knowledge on how to safely deal with a yeast infection during your period.
A yeast infection on your period — name a more uncomfortable and annoying duo. We’ll wait.
It’s bad enough to get an itchy yeast infection at any time of the menstrual cycle. But when coupled with your period, you wonder how long can you wear a tampon before things get really uncomfortable. The different products we use to manage our periods have the potential to cause further irritation to the vagina and/or vulva.1
What is a vaginal yeast infection, though? If you’re one of the lucky few who has yet to experience one, here’s a quick explanation:
A yeast infection, aka vaginal candidiasis, is a fungal infection that affects the tissues around the vulva and vaginal area.2 Over 75 percent of people with vaginas experience yeast infections in their lifetime. Yeast infection symptoms include intense itching in the vagina and vulva, and a burning sensation during intercourse or peeing. Sometimes redness or a thick, white, odor-free vaginal discharge that looks like cottage cheese — apologies for that visual.
Although yeast infections can be sexually transmitted, it is not considered a sexually transmitted infection (STI).
Yeast infections can be easily confused with bacterial vaginosis (BV), since they both cause itching, however, are typically odorless and typically accompanied by a thick, white discharge similar to cottage cheese. Bacterial vaginosis in the other hand, presents a foul-smelling fishy odor with thin, gray or white vaginal discharge.
Yeast infections tend to crop up when the precariously balanced ecosystem of vaginal microorganisms gets disrupted. In a “perfect” vaginal world, you have enough good bacteria in the vagina (i.e lactobacillus) to feed on yeast (i.e. candida albicans) populations and keep them under control. Having yeast in the vagina is normal, it’s just the overgrowth of yeast that causes an infection to occur.
When you’re pregnant or taking antibiotics, these populations can sometimes get a little bit out of hand, turning into a yeast overgrowth. Individuals with diabetes, a compromised or weakened immune system, or those using hormonal contraceptives such as the ring or birth control pills are also more prone to candida overgrowth.2 That’s usually when symptoms of a vaginal yeast infection start, and realize it’s time to pick up some Monistat (miconazole) ointment (or any other over-the-counter medications that can be used to treat a yeast infection, such as Vagistat (tioconazole), and Canesten (clotrimazole) or other antifungal medication), stat.
So, do tampons have an impact on recurring yeast infections? And how do you deal with it during your period? Dr. Jane van Dis, a board-certified OB-GYN with 13 years of experience, helps us answer those questions.
Tampons & recurring yeast infections: What’s the deal?
If you’re a tampon user who gets frequent yeast infections, you might wonder if there’s any correlation. This is especially true if the infections tend to show up during or around menstruation. Here’s what the science tells us:
A 2011 study published in the American Journal of Public Health, showed no correlation between types of menstrual products and more frequent yeast infections.3 The same study also found no correlation between yeast infections and tight clothing, diet, synthetic underwear, or feminine hygiene sprays.
So, tampons don’t cause yeast infections directly, nor is it unsafe to use them when you have one. However, there’s a chance they could increase your discomfort. Tampons have been associated with changes in vaginal mucous. In some cases, they’ve also been linked to vaginal ulcerations when used heavily or changed frequently.1
Any materials that are not biologically inert can interfere with your vagina’s delicate balance of yeast and bacteria.4 What’s ‘inert’ mean? Basically, it’s any material that doesn’t cause a response when introduced to biological tissue such as your vaginal walls.
When shopping for period products, take a moment to read the ingredients on the box. Absorbent materials like cotton and other natural or synthetic fibers are more likely to disrupt the vaginal mucosa. 1
Synthetic fibers may also release toxins into your bloodstream via your vagina’s highly vascularized walls.5 Inert materials, on the other hand, have no effect on vaginal flora or pH.
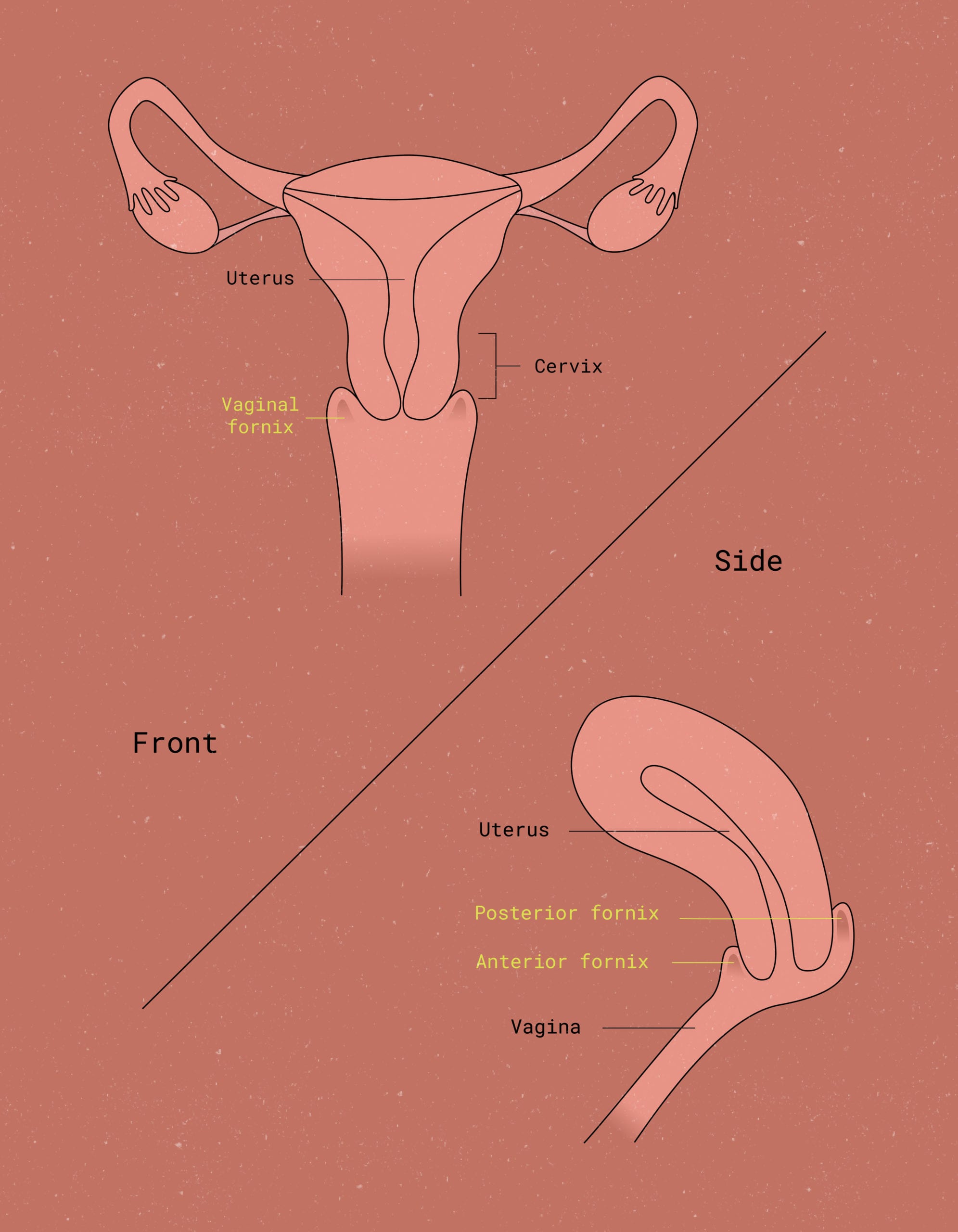
Dr. Jane says, “While it’s safe to use tampons when you have a yeast infection, it may not be comfortable. If I had a choice between a tampon and the Flex Disc™, I would choose the disc because it’s not a paper product, but [is made of] inert materials that don’t interact with the vaginal flora.” Flex® = less itchy messes. It also means less awkward movements in public when you’re trying to sneak a discreet scratch to your crotch area.


How to treat a yeast infection during your period
Battling a yeast infection on your period? You might be wondering how to treat it when you already have a lot of, um, fluid going on down there.
But can you use monistat on your period (aka miconazole nitrate)?
Yes, you can!
“Women [and non-women with periods] can still use antifungal vaginal preparations during their period,” Dr. Jane notes. “I would recommend placement at night right before bed.”
It may seem silly to use a vaginal suppository when your vagina feels like a bloody slip and slide. However, it can still be effective. By putting it in right before bed, gravity won’t interfere with the medication doing its job.
If more traditional antifungal yeast infection medications aren’t helping, you can also try boric acid suppositories. Clinical studies have found boric acid to be successful in treating candidiasis when other methods have failed.6 Note that boric acid should not be used if you are pregnant.
However: Don’t use vaginal suppositories (of any kind) with a tampon, since tampons will absorb some of the medication and prevent it from working as well.7 You may also want to avoid using menstrual cups, since the ingredients in the suppository could damage the cup’s materials. Stick with breathable, reusable period underwear, menstrual discs, or pads while using vaginal suppositories to treat a yeast infection.
Alternatively, your doctor may prescribe a one-time oral medication, such as fluconazole. Fluconazole, however, is contraindicated during pregnancy.
If you use pads, make sure to change them frequently. Yeast thrives in high-moisture environments. 8. You can help your body fight off a yeast infection by giving your vagina room to breathe. In other words, going about your day with a soaked pad or pair of period underwear may be counterproductive.
One study even found a correlation between frequent sanitary pad use and a higher risk of yeast infections. So, pads could be more likely to trigger yeast infection in the first place.9
Most people should be able to treat yeast infections during their period at home, per Dr. Jane’s recommendations. But if you don’t see results from at-home yeast infection treatments, it’s a good idea to talk to your doctor.
Please note that, if your yeast infection is due to a type of yeast other than Candida albicans, your doctor might recommend alternative medications like nystatin, or flucytosine, which are available as vaginal suppositories. Contrary to information you might have encountered online, there is no proof that home remedies such as tea tree oil, coconut oil, or probiotic supplements can effectively treat yeast infections.
Yeast infection on period: The right period product changes everything
If it seems like you always get yeast infections around your period, hormones (rather than tampons) may be the culprit. Dr. Jane explains, “Hormonal fluctuations preceding mensesAnother term for menstrual flow (commonly known as your period). and during mensesAnother term for menstrual flow (commonly known as your period). can lead to changes in vaginal pH and levels of ‘good bacteria,’ or vaginal flora.” In some individuals, these hormonal changes cause yeast populations to grow – and, voila, you have a yeast infection.
Using the right period products can help manage itchiness and discomfort. Menstrual discs and cups made of inert materials won’t mess with your vagina’s bacterial ecosystem. The same is true for most externally-worn period products, such as pads or period underwear. As long as they’re changed frequently, these should be fine.
Tampons trap moisture, so they may not be the best choice during a yeast infection. However, they haven’t been shown to actually cause yeast infections. Keep in mind that many tampon brands are made of synthetic materials. These synthetic materials could potentially release toxins into your bloodstream, disrupt the balance of bacteria, and create an environment favorable to the uncontrolled growth of yeast.5
Never leave a tampon in for longer than 8 hours. If you experience a sudden high fever, drop in blood pressure, vomiting, or diarrhea, seek medical attention immediately. These could be signs of Toxic Shock Syndrome (TSS), a potentially fatal illness.10
As always, talk to your healthcare provider if you experience recurrent yeast infections, severe pain, vaginal inflammation, or any other unusual symptoms. They will be able to provide qualified medical advice, diagnosis or treatment options.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2025 The Flex Company. All Rights Reserved.
- Friedrich, E. G. (1981). Tampon effects on vaginal health. Clinical Obstetrics and Gynecology, 24(2), 395-406. doi:10.1097/00003081-198106000-00007[↩][↩][↩]
- Yeast infection (vaginal) – Symptoms and causes. (2019, July 16). Mayo Clinic. Retrieved from mayoclinic.org/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999[↩][↩]
- Foxman, B. (1990). The epidemiology of vulvovaginal candidiasis: Risk factors. American Journal of Public Health, 80(3), 329-331. doi:10.2105/ajph.80.3.329[↩]
- Nowak-Sadzikowska, J., Bulanda, M., & Heczko, P. B. (1994). Wpływ tamponów dopochwowych na flore bakteryjna dolnego odcinka dróg rodnych [Effect of vaginal tampons on bacterial flora of the lower genitalia]. Polski tygodnik lekarski (Warsaw, Poland: 1960), 49(8-9), 207–209[↩]
- Nicole, W. (2014). A question for women’s health: Chemicals in feminine hygiene products and personal lubricants. Environmental Health Perspectives, 122(3). doi:10.1289/ehp.122-a70[↩][↩]
- Keller Van Slyke, K., Michel, V. P., & Rein, M. F. (1981). Treatment of vulvovaginal candidiasis with boric acid powder. American Journal of Obstetrics and Gynecology, 141(2), 145-148. doi:10.1016/s0002-9378(16)32581-9[↩]
- Vaginal Suppositories: How to Use Them. (2017, May 22). Healthline. Retrieved from healthline.com/health/general-use/how-to-use-vaginal-suppositories[↩]
- Usher, M. B., & Stoneman, C. F. (1977). Folsomia Candida – an ideal organism for population studies in the laboratory. Journal of Biological Education, 11(2), 83-90. doi:10.1080/00219266.1977.9654123[↩]
- Leegaard, M. (1984). The incidence of candida Albicans in the vagina of “Healthy young women”: How often do they have symptoms? Possible etiological factors. Acta Obstetricia et Gynecologica Scandinavica, 63(1), 85-89. doi:10.3109/00016348409156280[↩]
- Toxic shock syndrome – Symptoms and causes. (2020, March 18). Mayo Clinic. Retrieved from mayoclinic.org/diseases-conditions/toxic-shock-syndrome/symptoms-causes/syc-20355384[↩]