Uterine fibroids: Symptoms, diagnosis, and prevention
The lowdown on uterine fibroids (plus prevention tips)
If you have a uterus, you have a 70 to 80% chance of developing uterine fibroids at some point in your lifetime. Don’t freak out, though: Most uterine fibroids are asymptomatic and only cause for concern when they result in painful or otherwise inconvenient symptoms.
Understanding the what, how, and why behind this condition is critical for keeping an eye on your body’s overall wellness.
What are uterine fibroids (leiomyoma)? And what causes them?
In most cases, uterine fibroids are benign. They are solid, compact, non-life-threatening tumors made of fibrous connective tissue and muscle cells commonly found inside the uterine wall. There is a 70-80% chance you will have one in your lifetime.
Although fibroids are technically tumors, they are usually non-cancerous and have not been proven to increase the risk of cancer of the uterus. However, these fibroids, also known as leiomyoma and myoma, sometimes cause excessive vaginal bleeding or discomfort. Treatment may result in a myomectomy, which is a surgical procedure to remove the fibroid.
As common as fibroids are, only one-third grow large enough to be detected by a doctor during a routine exam. They can be as large as a grapefruit or as small as a pea.
Are there different types of uterine fibroids?
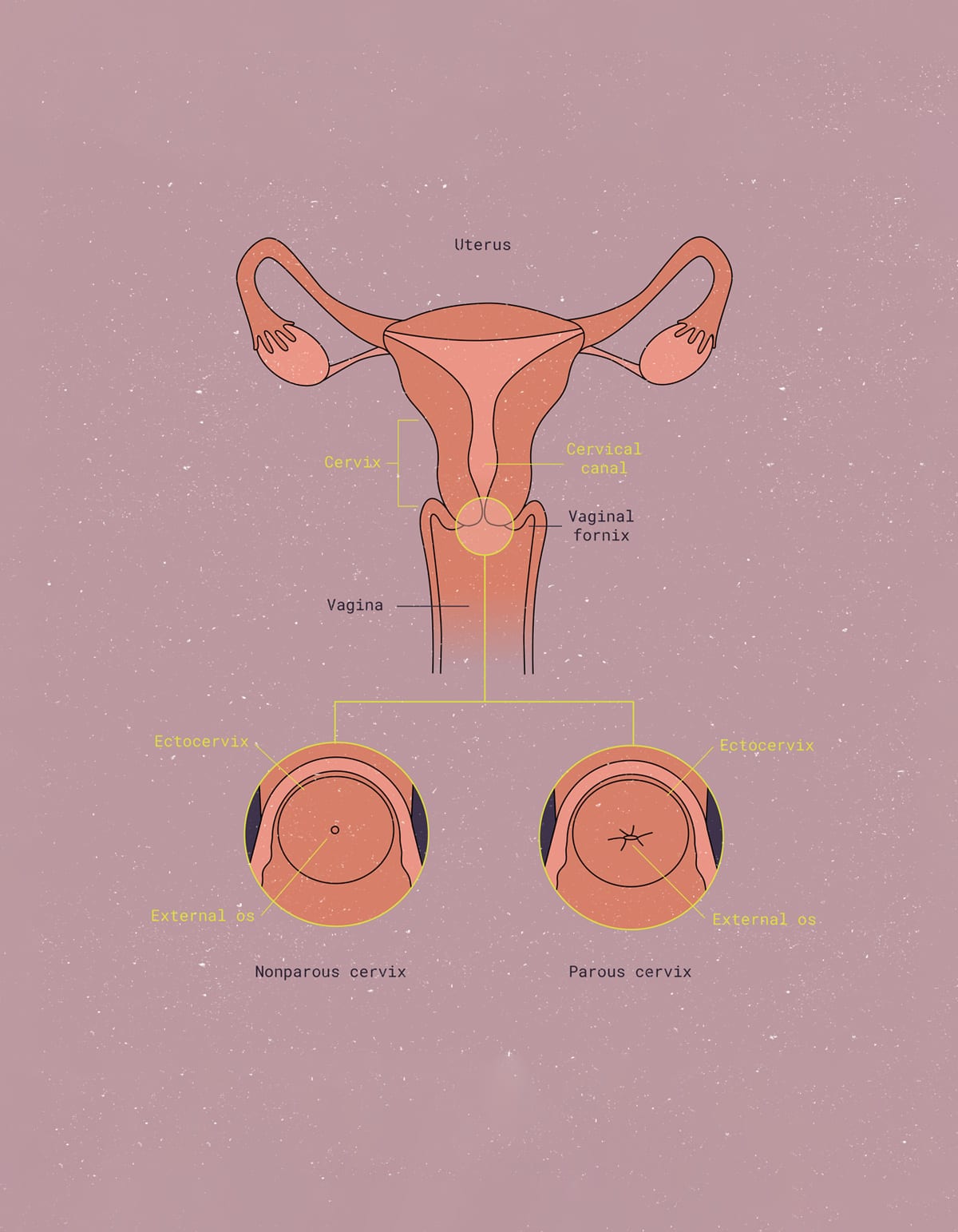
Fibroids are generally classified by where they grow within or around the uterine cavity. Depending on the location of the fibroids, there are several types of uterine leiomyoma:
1. Intramural fibroids
These grow within the walls of your uterus and, at their worst, can grow to stretch the womb. These are one of the most common forms of uterine fibroids. Depending on where they are located in the uterus, they can be anterior intramural fibroids, posterior intramural fibroids, or fundal intramural fibroids.
2. Subserosal fibroids
They grow on the outside of the uterus and sometimes expand to make the womb appear larger on one side. These can cause pressure or discomfort in the pelvic area or lower back. They can also cause urinary and digestive issues if they press against the bladder or intestines.
3. Submucosal fibroids
They project inwards, towards the uterine cavity. Submucosal fibroids have been linked to impaired fertility and can cause prolonged and heavy periods. When a submucosal fibroid protrudes into the uterine cavity, it can lead to complications such as miscarriage or difficulties in conceiving.
4. Pedunculated fibroids
They form when subserosal fibroid tumors develop a stalk, or pedunculate, that projects into the inside part of the uterus and can cause severe pain and discomfort. These types of fibroids can sometimes twist on their stalk, leading to further complications and requiring immediate medical attention.
Uterine fibroids: Prevalence and risk factors
Certain demographics and characteristics put some individuals at higher risk of developing fibroids. These include:
- Race – African-American women are at a higher risk of developing fibroids, more than women of other ethnic groups. Black women are also more likely to develop more leiomyomas at a younger age, in higher quantities and greater size of the tumor.
- Heredity – A family history of uterine fibroids increases personal risk.
- Early menopause – People approaching menopause experience extended periods of high estrogen levels, which has been linked to the growth of fibroids.
Researchers are investigating possible links between fertility and uterine fibroids, as the tumors tend to appear less frequently in women who have early pregnancies.
How can I prevent uterine fibroids?
Because the exact cause of uterine fibroids remains unknown, healthy lifestyle choices remain the best preventative care. Some evidence links exercise to a lowered risk of developing uterine fibroids, possibly because exercise helps to stabilize insulin and sex hormone levels.
Scheduling routine pelvic exams and checkups with your primary care physician or gynecologist can help you detect early fibroids and determine the best treatment method.
Symptoms of uterine fibroids
Most people will not notice their presence – for some, however, these small tumors can bring varying degrees of complication or discomfort. Here are some of the most common symptoms of fibroids:
Pain and discomfort:
Pelvic pain is particularly common if the myoma tumor grows large enough to press on pelvic organs such as the bladder or intestines. This sometimes manifests as abdominal pressure or a sense of fullness or bloating in the stomach area. It can also cause a feeling of heaviness in the pelvic area.
Irregular periods:
Uterine fibroids can impact the menstrual cycle, leading to heavy menstrual bleeding, prolonged periods, bleeding between periods, blood clots, and sometimes anemia, even anemia requiring blood transfusion. They can also cause menstrual cycle irregularity.
High blood pressure:
Individuals diagnosed with fibroids are at risk of high blood pressure (hypertension) and heart disease.
Other symptoms:
People with fibroids can experience mild to severe symptoms. Lower back pain, painful intercourse, frequent urination, constipation or incontinence, and anemia. In addition, some women report feeling fibroids externally. They can sometimes appear as firm masses near the center of the pelvis.
Potential risks & complications
They generally don’t require any medical attention, but if they continue growing, they can lead to long term or intensified discomfort. Fibroids grow by seizing the blood vessels that supply nearby organs. Once they outgrow or deplete their blood flow, larger fibroids will start to die on their own.
Your doctor may want to monitor the development of the leiomyoma, as rapid growth may be a sign of a rare cancerous fibroid, leiomyosarcoma. Their continued growth can also lead to prolonged or intensified discomfort, requiring removal.
Some studies indicate that some fibroids can affect fertility. Submucosal fibroids are especially susceptible. These tumors sometimes cause recurrent miscarriages, and if this is the case, they likely will need to be surgically removed in order to carry a pregnancy. See your doctor if this is a potential concern.

Uterine fibroid treatments & diagnosis
Talk to your gynecologist about including a pelvic exam for uterine fibroids during your next routine checkup. If you are concerned that you may have a fibroid, your provider may schedule an ultrasound or an MRI (magnetic resonance imaging) guided exam following a regular pelvic exam.
In addition, people experiencing challenges in becoming pregnant may be eligible for either hysterosalpingography (a form of x-ray used to examine the uterus and fallopian tubes and investigate miscarriages) or a diagnostic hysteroscopy to take a look inside the uterus with a small camera.
Most fibroids will stop growing or shrink on their own. If you do have one, your doctor will likely first monitor the fibroid growth before scheduling treatment or removal.
Uterine fibroids treatment options include a variety of non-surgical options as well as surgical procedures, including uterine fibroid surgery, commonly known as a myomectomy. The following treatments aim to reduce pain and discomfort as well as decrease their blood supply:
- Over-the-counter pain medication, such as ibuprofen
- Oral contraceptives (i.e. birth control pills)
- Iron supplements
- Choosing period products that accommodate heavier menstrual flow, such as a menstrual cup or menstrual discs
In addition, and depending greatly on the nature of your fibroids, your provider might consider:
- Selective Estrogen Receptive Modulators (SERMs) – A type of medication that works on your estrogen levels and may reduce their size without causing menopause-like symptoms.
- Gonadotropin-releasing hormone agonists (GnRH therapy) – Gn-RH is a hormone naturally produced by the brain’s hypothalamus. When Gn-RH agonists are introduced as therapy, estrogen, and progesterone levels fall, menstruation stops, anemia improves and fibroids shrink. This is basically termed a short-course “medical menopause” because the side effects of the Gn-RH agonists mimic those of natural menopause (hot flashes, vaginal dryness)
- RU-486 (the abortion pill) – Currently being researched and tested as a form of treatment. The abortion pill has been shown to reduce the size of the fibroids by up to 50%.
- Depo-Provera – Depo-Provera is a progesterone-like injection normally used to prevent pregnancy and sometimes used to treat myoma. It decreases the size of the lining of the uterus, thereby reducing heavy bleeding and tissue size.

Finally, in rarer cases, surgeries and procedures may be considered including the following:
- Uterine Artery Embolization (UAE) – In UAE, an x-ray is used in conjunction with a catheter to deliver particles that block the uterus’s blood supply. It has been proven to reduce the size of fibroids with a 90% success rate.
- Endometrial ablation – A procedure that destroys a thin layer of the uterine lining, while reducing menstrual bleeding to normal levels. Side-effects may include cramping and frequent urination.
- Myomectomy – Unlike a hysterectomy, a myomectomy removes the symptom-causing fibroids and leaves the uterus intact. Myomectomy is the preferred choice for women who still plan to have children. Depending on your specifics, the doctor may either recommend a hysteroscopic or an abdominal myomectomy. Abdominal myomectomy accesses the fibroids through small incisions in the abdomen, while in a hysteroscopic myomectomy, the surgeon removes them by inserting a hysteroscope into the uterine cavity through the vagina and cervix. While myomectomy is often a safe, low-risk procedure, rare cases of complications in this type of surgery can result in a need for a hysterectomy.
- Hysterectomy – A hysterectomy is the complete removal of the uterus. This may be the best option for menopausal women or women who do not plan to have children.
Fibroid misdiagnosis & other growths to be aware of
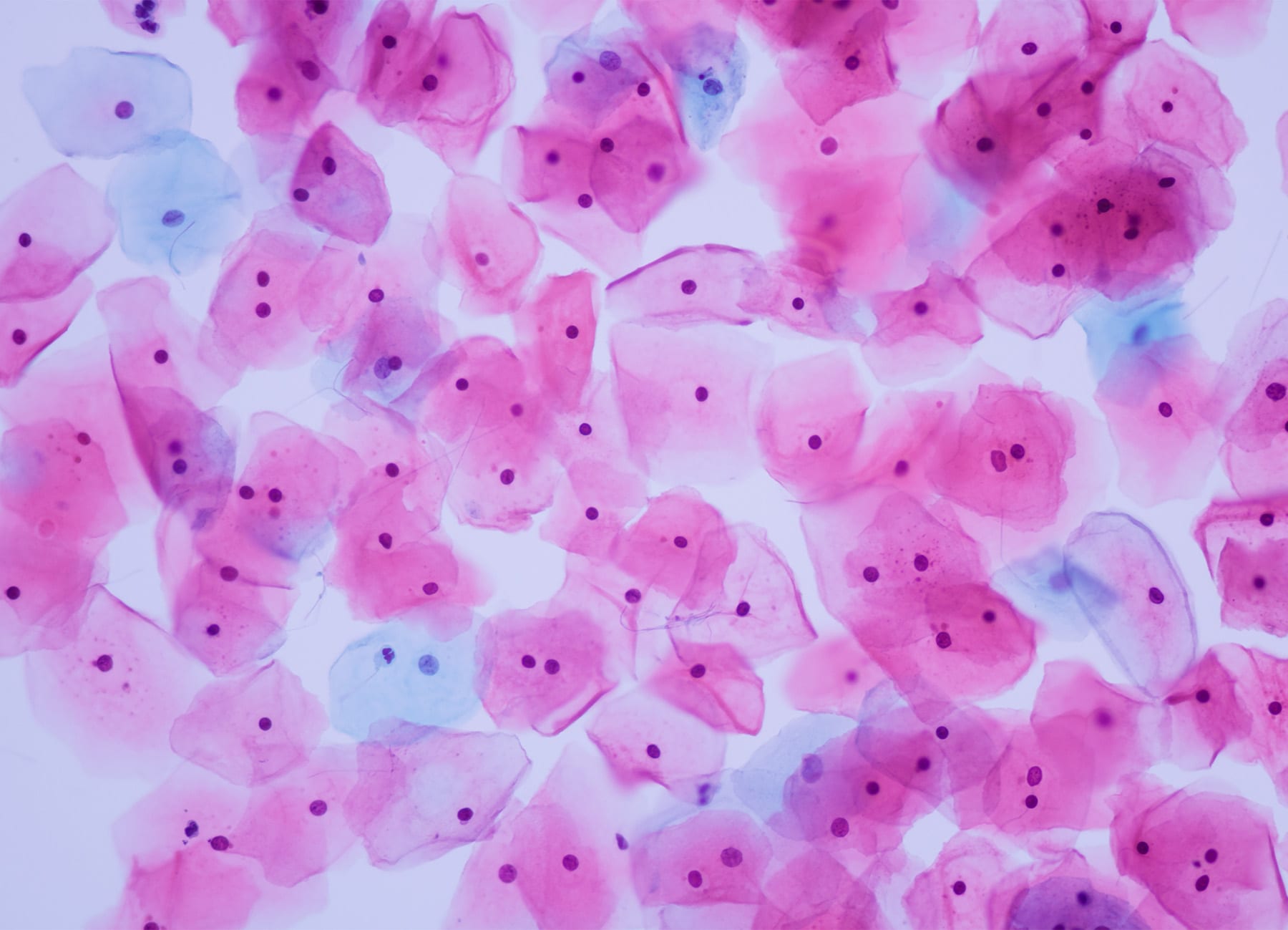
While fibroids are a growth formed from muscle tissue, polyps are an overgrowth of uterine tissue within the uterine cavity. Fibroids are benign, but polyps can be cancerous.
Both cause similar abnormalities in menstruation and result in some similar symptoms. Because they also look similar in an ultrasound, polyps are sometimes misdiagnosed as fibroids.
The best way to diagnose a malignant polyp is to remove it and send the polyp to a pathologist for routine testing.
Continued research & preventative health measures
Researchers are still growing their understanding of the possible causes of uterine fibroids, but experts are certain that most of these benign tumors are no cause for alarm.
Making responsible choices in eating a healthy diet and participating in regular exercise can have lifelong benefits that may help combat fibroids or prevent uterine leiomyoma.
Talk to your general practitioner about the risks of uterine fibroids and make sure to schedule routine checkups to be safe. If you have a fibroid, talk to your provider about different treatment plans to alleviate any pain or discomfort.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2024 The Flex Company. All Rights Reserved.