IN THIS ARTICLE
The medical definition of “spotting”
There’s nothing like those “not-quite-your-period-but-still-bleeding” moments to throw you off your game. Spotting is a common medical phenomenon—but it tends to have the worst timing.
While spotting isn’t the same thing as your normal period in full force, it’s an equally important indicator of your health. In some cases, it can point to an underlying condition. In other cases, it’s just a completely harmless, random annoyance. That’s why it’s so important to be aware of what causes it (as well as the related signs or symptoms to look out for).
What is spotting?
Spotting, sometimes called “intermenstrual bleeding,” refers to vaginal bleeding that occurs between your regular menstrual periods.1 In other words, is the bleeding that happens at a point during your cycle when you wouldn’t necessarily expect it (such as during the luteal phase or around ovulation).
While some people refer to the lighter days at the end of menstruation as “spotting,” those instances don’t actually qualify. If it happens around the end or the start of your period, it’s probably just… light period bleeding.

Here’s how to tell the difference between spotting and period
Most menstruators get a regular period about every 28 days—during those 28 days (regular cycle), your body goes through all four stages of the menstrual cycle.2 During menstruation, your levels of estrogen and progesterone plunge, prompting the top layers of your thickened uterine lining to shed. On average, you’ll lose about 30 to 80 mL of menstrual blood during a period.1 That translates to somewhere between 6 and 16 teaspoons of period blood.
Still, according to a study published in the BMJ, about 36% of people with periods who report to primary care providers with menstrual problems have intermenstrual or post-coital bleeding in addition to heavy menstrual flow.3
Unscheduled, irregular bleeding, unlike your period, does not happen cyclically. It can occur:
- In between normal menstrual periods
- Before puberty
- After menopause
- During or after sexual intercourse
Spotting can also be characterized by the amount of blood that shows up in your underwear (or toilet paper); it should not cover or soak through a panty liner.4
Sometimes, it can be difficult to pinpoint if your periods are irregular or just very light periods. While there are many innocent causes of spotting, there are also a handful of more serious conditions that bring about those “random” drops of blood that make you break out that stain remover to salvage your favorite pair of underwear.
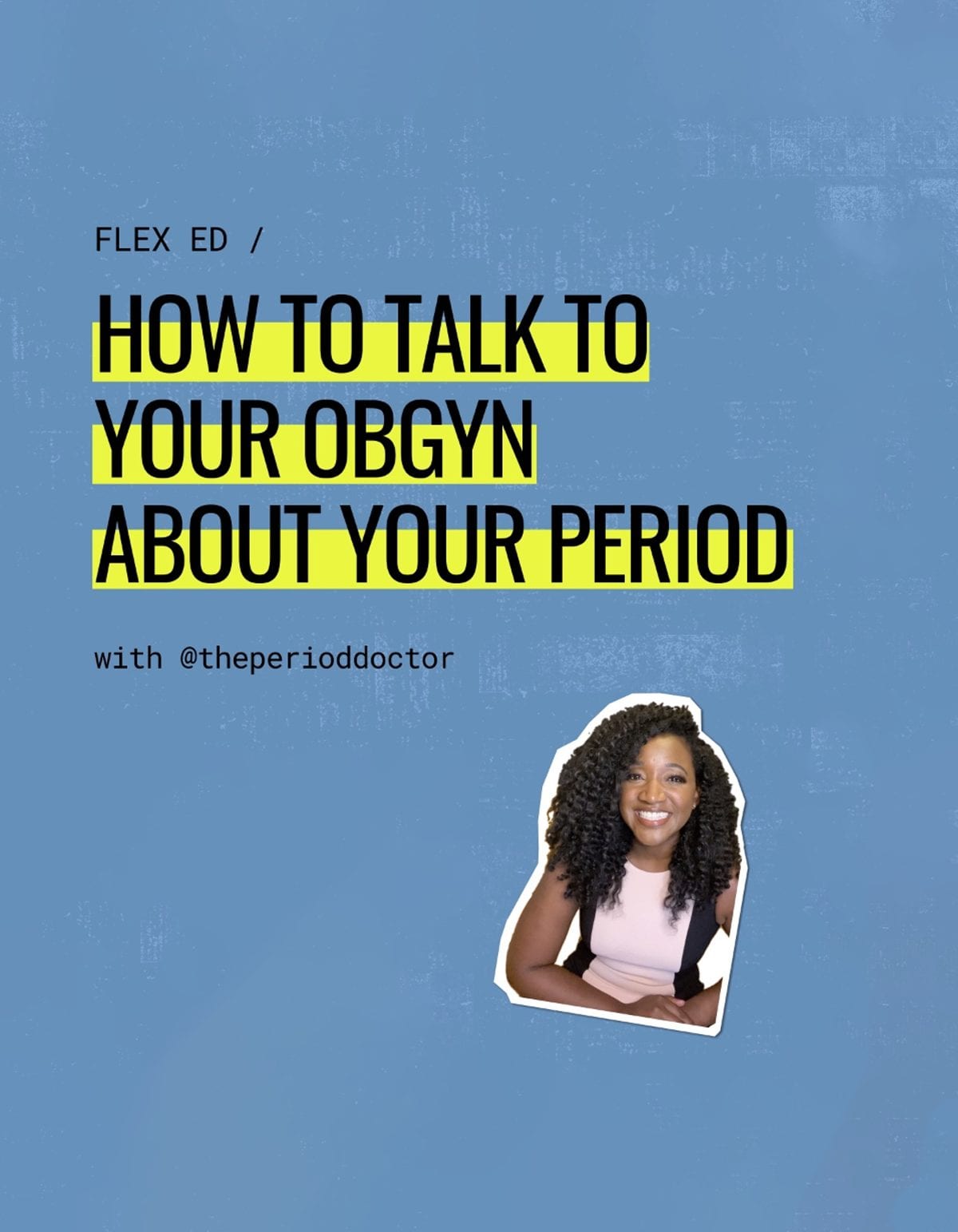
If you’re unsure whether your vaginal bleeding is due to your period or just an unexplained occurrence, talk to your health care provider or OB/GYN.
Why spotting happens: Common causes
As mentioned above, spotting may catch you off-guard, but it’s pretty common—and its possible causes can range from gynecologic to hormonal to stress-related.
One especially common reason for spotting is starting a new form of birth control, like the pill, patch, or IUD. To learn more about how hormonal contraceptives can affect your period and/or spotting, read all about birth control bleeding here.
Some menstruators may also experience age-related spotting. Maybe you’ve just started getting your period, in which case light or irregular vaginal bleeding is normal, or maybe you’re entering into perimenopause (which typically happens if you’re in your forties or fifties).5
Here are a few (but not all!) of the possible causes:
There are many different reasons why you could be spotting. Possible causes:1
- Stress
- Uterine fibroids
- Endometriosis
- Cervical or uterine polyps
- Hormonal changes
- Inflammation or infection of the cervix (cervicitis) or uterus (endometritis)
- Vaginal injury or trauma
- Some Sexually Transmitted Infections (STI’s) like Gonorrhea and Chlamydia if not treated on time can cause vaginal bleeding, along with pelvic pain
- Polycystic Ovary Syndrome (PCOS)
- Pelvic Inflammatory Disease (PID)
- IUDs, or using hormonal birth control irregularly (such as stopping and starting or skipping birth control pills, patches, or estrogen rings)
- Ectopic pregnancy, miscarriage, or other pregnancy complications
- Vaginal dryness due to lack of estrogen after menopause
- Underactive thyroid (low thyroid function)
- Certain medications such as Hormone Replacement Therapy.
- Some people notice light spotting after a pelvic exam or a pap smear.
The important takeaway here is that spotting can be caused by lots of different things going on in your body—from medication to stress to injury, inflammation, or could be sign of an underlying condition.
Spotting doesn’t always spell trouble, in some cases it can even be expected. Conversely, there are also situations where it can be a cause for greater concern and something worth discussing with your primary care physician or OB/GYN.

Different types of spotting and what they could mean
There are many different types of spotting that occur in specific circumstances. Here are a few benign types of spotting to look out for if you happen to be:
- Tracking your menstrual cycle,
- are trying to get pregnant,
- are using hormonal contraceptives,
- or are approaching menopause
1. Ovulation spotting
Ovulation = the phase of the menstrual cycle during which your ovary releases an egg. However, the ovulation process begins earlier than the actual egg release. Typically lasting between 16 to 32 hours in total, ovulation technically begins when the body experiences a spike in luteinizing hormone levels (LH).6
Spotting during the ovulatory phase of your menstrual cycle is uncommon but not unheard of, and it may be connected to higher estrogen levels experienced during this phase. In one study, nearly 5% of participants reported an instance of unexplained spotting—lasting on average between one and two days—around or during ovulation.7 Translation? It’s not the most typical cause for spotting, but in most cases, it’s probably harmless.
Note here that ovulation does not equal fertile window. Your fertile window starts in the five days leading up to ovulation, plus the day of ovulation and the day after ovulation. This is the time when pregnancy is most likely to occur if you are trying to conceive. Ovulation spotting, while relatively uncommon, can sometimes be an indicator of your most fertile days during this window.
However, if you experience spotting outside of your menstrual cycle or in conjunction with other symptoms like severe abdominal pain, unusual or bloody vaginal discharge, or fever, it’s essential to consult with a healthcare provider promptly. These could be signs of underlying issues that require medical attention to diagnose and treat effectively.

2. Implantation bleeding: Pregnancy Spotting vs Period
Pregnancy tends to be a wonderful and also super-stressful time. And spotting or light bleeding during pregnancy can turn those stress levels up to 100, especially if the cause is unknown.
Rest assured: While it can be unsettling to notice those small amounts of blood, ~20% of people who experience spotting while pregnant go on to have a healthy pregnancy and baby.8 There are several situations during pregnancy where spotting is commonly seen.
One of these instances—implantation bleeding—occurs in the first trimester, when the fertilized egg attaches to the lining of your uterus.4 This type of spotting can occur in early pregnancy, when the embryo implants and begin to grow in the womb and before you even know you’re pregnant, and may last up to a few days.
If you’re experiencing unscheduled bleeding and are unsure if you may be pregnant, take a home pregnancy test or consider speaking to your primary care physician or OB/GYN as it may be one of the very first symptoms of pregnancy.
Other symptoms of pregnancy include nausea, breast tenderness, fatigue, and a missed period. It’s important to remember that every pregnancy is unique, and not everyone will experience the exact same symptoms or level of spotting.
Other pregnancy-related spotting
These can occur due to cervical polyps, which is a relatively harmless growth on the cervix. Polyps are more likely to grow (and thus bleed) during pregnancy.9
Always speak to a medical provider if you’re unsure about the cause. While spotting during pregnancy is not always a medical emergency, there are cases where bleeding while pregnant can be a sign of a more serious illness, especially in the second and third trimesters. Any bleeding, especially after the first trimester, should be reported to your obstetrician.9

3. Breakthrough bleeding (birth control spotting)
Another common cause has to do with being on birth control—in these cases, it’s also known as breakthrough bleeding. This is a common side effect in those who’ve recently started hormonal birth control methods (including the pill, patch, ring, or hormonal IUD). Unscheduled bleeding or light spotting on birth control can also occur if you take birth control pills irregularly or skip placebo pills.
4. Spotting during perimenopause
Perimenopause is the timeframe when people AFABAFAB stands for “assigned female at birth.” near menopause – marking the end of their reproductive years. This typically occurs in your 40s, however, some women experience changes in menstrual regularity as a result of perimenopause as early as their mid-thirties.10
In a study of perimenopausal people, 24% reported an instance of intermenstrual bleeding. In perimenopausal people, there is a higher prevalence of both spotting in between periods and after sex. 11 Even with menstrual irregularity, it’s important to discuss any abnormal vaginal bleeding such as extremely heavy bleeding, extended bleeding over seven days, excessive, persistent spotting, or periods occurring less than 21 days apart.10
How to manage spotting: What products to use
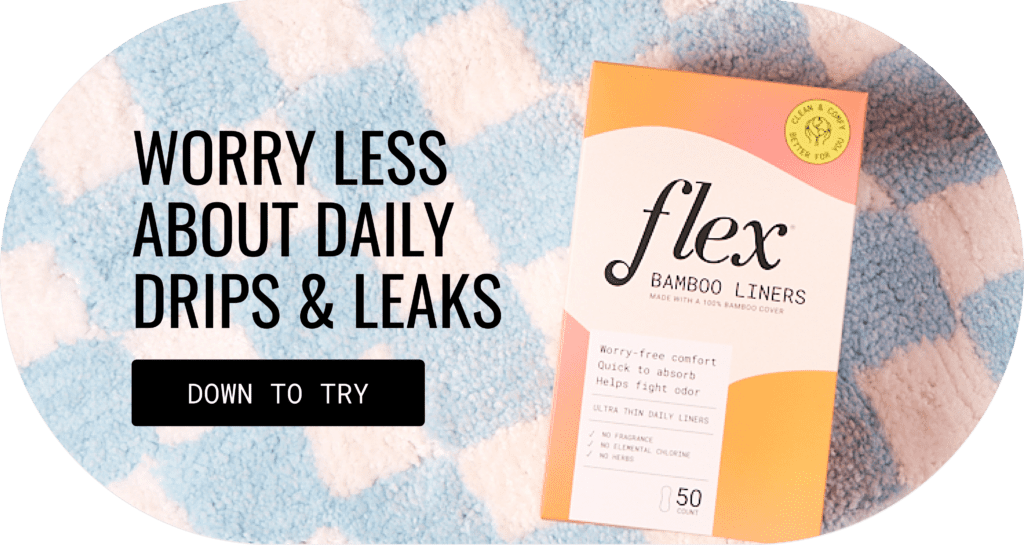
Spotting can be super frustrating—especially when it happens, like magic, on the exact day you chose to wear a brand new pair of white underwear from your favorite brand. Thankfully, there are period products you can use safely for spotting to help protect your clothes (or sheets) from unscheduled bleeding.
Liners are a great option to use while spotting. Since they’re thinner and more compact than regular pads, you can stash them easily in your bag (or even in your wallet) in case you have an unexpected emergency.
A menstrual disc is another great choice for spotting, especially if it’s recurrent—like when you’re transitioning onto a new form of hormonal birth control. Flex Disc is made from body-safe, medical-grade polymers that glide in and out comfortably even when there isn’t a whole lot of lubrication in the vaginal canal (so you can say goodbye to that cringey dry tampon removal).

Pads and tampons are popular period products. Pads are a good idea, but using tampons for spotting can actually increase your risk for bacterial infection.
Spotting vs. your period: Key takeaways
Your menstrual cycle doesn’t end when your period does. Your reproductive system stays in flux and it’s important to keep track of any unexpected changes in your typical menstrual cycle.
If you’re unsure how to approach this topic with your primary care physician or OB/GYN, here are some possibilities to consider:2
- If there is a chance you might be pregnant
- How long has the spotting persisted
- If there are any other associated symptoms (cramping, pelvis pain, etc)
- If you are taking any medications
- If you have missed your period or had a heavier or irregular period or abnormal bleeding
- What does your spotting look like
Spotting can be bothersome, but understanding and taking note of changes in your reproductive health can help you spot potential problems earlier—and, at the very least, might save you from another pair of stained underwear.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2025 The Flex Company. All Rights Reserved.
- Medline Plus. (2019, March 28). Vaginal bleeding between periods. Medline Plus. https://medlineplus.gov/ency/article/003156.htm[↩][↩][↩]
- Healthgrades Editorial Staff. (2021, January 8). Spotting. Healthgrades. https://www.healthgrades.com/right-care/womens-health/spotting[↩][↩]
- Warner, P., Critchley, H. O., Lumsden, M. A., Campbell-Brown, M., Douglas, A., & Murray, G. (2001). Referral for menstrual problems: cross-sectional survey of symptoms, reasons for referral, and management. BMJ (Clinical research ed.), 323(7303), 24–28. https://doi.org/10.1136/bmj.323.7303.24[↩]
- Medline Plus. (2018, September 25). Vaginal bleeding in early pregnancy. Medline Plus. https://medlineplus.gov/ency/patientinstructions/000614.htm[↩][↩]
- Villavicencio J, A. R. (2016). Unscheduled bleeding and contraceptive choice: increasing satisfaction and continuation rates. Open Access J Contracept, n/a(n/a), 43-52. https://doi.org/10.2147/OAJC.S85565[↩]
- Knudtson, J., & McLaughlin, J. E. (2019, April). Menstrual Cycle. Merck Manual. https://www.merckmanuals.com/home/women-s-health-issues/biology-of-the-female-reproductive-system/menstrual-cycle [↩]
- Sonya S. Dasharathy, Sunni L. Mumford, Anna Z. Pollack, Neil J. Perkins, Donald R. Mattison, Jean Wactawski-Wende, Enrique F. Schisterman. (2012, March 15). Menstrual Bleeding Patterns Among Regularly Menstruating Women. American Journal of Epidemiology, 175(6), 536–545. https://doi.org/10.1093/aje/kwr356[↩]
- Warner, P., Critchley, H. O., Lumsden, M. A., Campbell-Brown, M., Douglas, A., & Murray, G. (2001). Referral for menstrual problems: cross sectional survey of symptoms, reasons for referral, and management. BMJ (Clinical research ed.), 323(7303), 24–28. https://doi.org/10.1136/bmj.323.7303.24 [↩]
- American Pregnancy. (2020, July 13). Spotting During Pregnancy. American Pregnancy. https://americanpregnancy.org/healthy-pregnancy/pregnancy-concerns/spotting-during-pregnancy/[↩][↩]
- Mayo Clinic Staff. (2020, December 21). Perimenopause. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666 [↩][↩]
- Shapley, M, Blagojevic‐Bucknall, M, Jordan, KP, Croft, PR. (2013, October). The epidemiology of self-reported intermenstrual and postcoital bleeding in the perimenopausal years. BJOG: An International Journal of Obstetrics & Gynaecology, 120(11), 1348-1355. 10.1111/1471-0528.12218 [↩]