Pelvic floor exercises to try at home
How to tone, stretch, and strengthen your pelvic floor muscles
Did you know that there’s an entire group of muscles that you’ve probably never “worked out” in your entire life—but that play a key role in things like having enjoyable sex (for starters!), using the bathroom, and staying balanced through your core?
Yep. Those specific muscles form a sling or hammock across your pelvic floor, and they get nowhere near as much attention as we think they should, especially in today’s conversations around women’s health and wellness. This lack of awareness runs in complete opposition to how common pelvic floor dysfunction is: It’s estimated to affect nearly one in four women in the United States.1 It can affect men, too, but it is significantly more common in people AFABAFAB stands for “assigned female at birth.”.
Whether you’re already well acquainted with pelvic health or if this is the first time you’ve ever heard of it, you’re in the right place. We’re sharing a few *super relaxing,* wellness-boosting pelvic floor exercises you can do at home (for free!) to help combat or prevent pelvic floor dysfunction.
As an added bonus? Working these exercises into your daily routine might not only help you improve your quality of life if you have PFD, but they can also even help you achieve some of the best orgasms of your life—and that’s something we can always get behind.2 3
Grab a mat or towel and let’s get started.
What’s pelvic floor therapy all about?
If you ask the average person what they know about pelvic floor physical therapy (PFPT), they might respond along the lines of, “Um… isn’t that, like, kegels?”
Yes! But there’s a lot more to it than PF contractions (a.k.a. kegels) and releases (a.k.a. reverse kegels).
PFPT is practiced to treat a range of PF disorders, but for the most part, they all can be classified under the blanket term, “pelvic floor dysfunction,” or PFD. A pelvic floor physical therapist might use a number of techniques to address PFD, ranging from strengthening exercises to manual therapy (i.e. hands-on stretching or massage), PF biofeedback, electrical stimulation(which uses mild electrical currents to stimulate pelvic muscles, which can help strengthen them or normalize nerve activity). They can also use myofascial acoustic compression therapy, which uses focused sound waves to target deep tissues and muscles to help relieve pain and tension. They can also use vaginal dilators.(2018, September 21). ISSM. https://www.issm.info/sexual-health-qa/what-is-pelvic-floor-physical-therapy/))
Wait a sec…what’s pelvic floor dysfunction?
If you missed our last article of this series, here’s a quick recap: Pelvic floor dysfunction (PFD) is a condition in which the pelvic floor is either chronically too tight or too weak, leading to impaired relaxation and coordination of your pelvic floor muscles.4 PFD can cause or exacerbate problems such as pelvic pain, urinary or fecal incontinence, difficulty eliminating urine, overactive bladder, trouble having bowel movements, pain during sex, and pelvic organ prolapse.1 Talk to your gynecologist if you experience any of these symptoms of pelvic floor dysfunction, and also have any of the previously mentioned conditions.
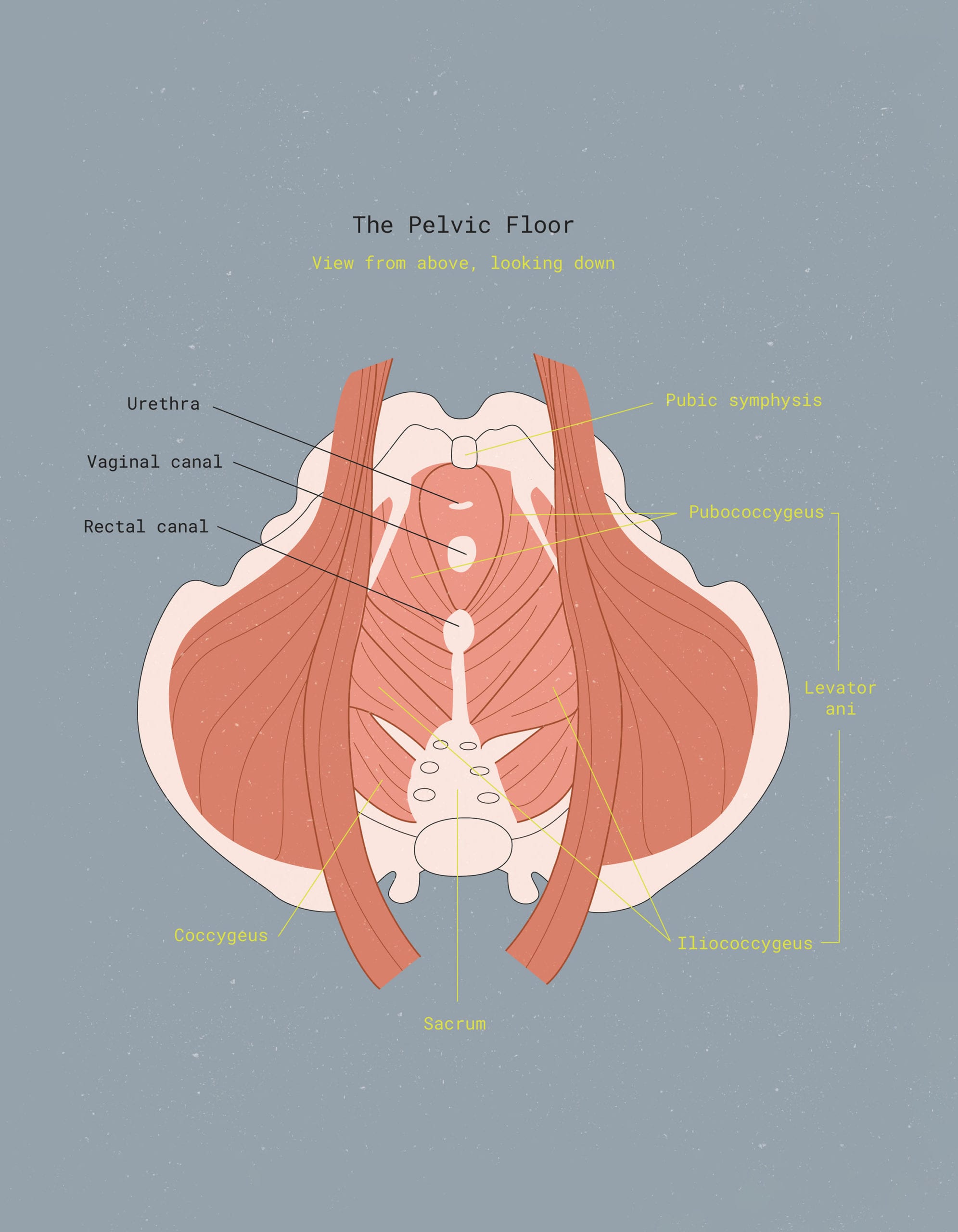
Your key pelvic floor muscles include the pubococcygeus, puborectalis, and iliococcygeus. Together, the pubococcygeus and iliococcygeus make up what’s called the levator ani.
In order to comfortably void waste (a.k.a. poop), your pelvic floor muscles need to be able to relax and lengthen “on command.” Same goes when having sex. If your pelvic floor muscles are unable to relax and tighten normally, you may experience constipation or diarrhea, difficulty emptying your bladder and bowel, pain or difficulty wearing certain period products (like tampons or a menstrual cup or disc), and/or the inability to orgasm.5

While there are a number of reasons why someone might develop PFD—including certain underlying illnesses, injury, obesity, menopause, or vaginal childbirth—many milder cases of dysfunction are preventable. And even those with severe symptoms of pelvic floor disorders can find a degree of relief by making lifestyle changes and practicing physical therapy.6
How does PFPT help with pelvic floor dysfunction?
When it comes to addressing PFD, you have a few options: Your best bet is, of course, always to start by talking to your healthcare provider. That way, you can work to address any underlying conditions that might be contributing to your symptoms, such as endometriosis, vulvodynia, or interstitial cystitis.
PFD and chronic pain tend to work in a sort of feedback loop, where pain makes your pelvic floor muscles tighter or more prone to spasm, which in turn causes more pain. That’s why it’s often recommended that patients treat any underlying chronic pain conditions with multiple modalities, including medication, diet, and PFPT (or other physical interventions).7
Once you’ve received a diagnosis and established an initial treatment option with your primary care provider or OB/GYN, you might consider reaching out to a pelvic floor PT who can provide hands-on assistance and create a custom treatment plan.
Along with showing you how to perform exercises (which may or may not include kegels) to help your pelvic floor, a PFPT might also provide external and/or internal (i.e. vaginal) manipulation to address muscle dysfunction precisely. This hands-on therapy might involve putting gentle pressure on a certain muscle to help release a trigger point or break up scar tissue.8
It might sound a little weird or awkward to think of a physical therapist sticking their fingers inside your vagina, but an experienced practitioner will know how to ease you into things and make sure you’re completely comfortable throughout your session. Internal manual therapy isn’t always necessary (and patients always have the option to decline it), but it can be super helpful when treating certain cases of PFD.
After your session with your PT, you’ll be given a series of exercises to practice at home. Most of which are typically stretching or strengthening exercises for your hips, core strength, and surrounding muscle groups—as well as (in some cases) kegels or reverse kegels. The exact set of exercises you’re given will depend on the nature of your PFD, i.e. whether you’re dealing with chronic over-tightness or spasming in certain pelvic areas, weakness, or a combination of the two.
On average, it takes somewhere between six to eight hour-long sessions with a pelvic floor therapist to treat myofascial pelvic pain or PFD. This timeframe can vary from person to person.6 Individuals with medical history of underlying chronic conditions may even choose to continue pelvic floor therapy indefinitely if their health coverage has no maximum limit.
In-person pelvic floor physical therapy vs. at-home exercises
Getting help from a trained pelvic floor physical therapist is the “gold standard” when it comes to treating chronic pelvic pain or PFD. Unfortunately, access to affordable PFPT varies from place to place, and your ability to see a physical therapist in person may depend on where you live and your health insurance coverage.
So, what if you can’t get in-person PFPT? Or what if your pelvic floor issues are pretty minor—like a little urine leakage here and there when you laugh too hard or occasional pelvic discomfort? Fortunately, there’s a LOT that can be done on your own—all from the comfort of your living room floor.
Even if your pelvic floor muscles seem to be doing just fine, working a few of these exercises into your daily routine may help to prevent pelvic floor issues like PFD and urinary incontinence in the long run.9 And don’t forget about the other benefits that come along with toned and healthy pelvic floor muscles…like improved sexual function, more pleasurable orgasms, a stronger core, and improved athletic performance, just to name a few.6 2
Before we dive in, we wanted to give a shoutout to our friends at Los Angeles-based Origin Physical Therapy for putting together this set of exercises for our readers to try. Visit Origin online or give them a call to learn more about their services (both virtual and in-person pelvic floor therapy appointments currently available).

Pelvic floor muscle exercises to try at home
Pelvic floor strengthening exercises:
1. Transverse Abdominal (TA) March:
Lie on your back with your knees bent and your feet flat on the floor. Find your “neutral spine” by rocking your pelvis backwards and forwards until you find your midpoint. Next, draw your belly button towards your spine (like you’re sucking it in to squeeze into a too-small pair of leggings).
Breathe normally. Hold this contraction and, while doing so, slowly raise one foot until your thigh is at a 90-degree angle to your spine. Exhale as you lift the foot up; inhale as you place it back on the floor. Repeat, alternating legs, for 1 minute.
2. Glute Bridges:
Lie on your back with your knees bent and your feet flat on the floor. Keep your hands by your sides with your palms facing down. Squeezing your glutes and pelvic muscles, exhale and press your hips up toward the ceiling, lifting your butt off the floor.
Don’t go too far – you don’t want to create an arch in your lower back. Pause for a breath or two at the top and then lower your pelvis back down to the floor on an inhale. Repeat for 8-12 reps.
3. Kegel exercises (a.k.a. Pelvic Floor Contraction):
To perform kegel exercises, lie on your back with your knees bent and your feet flat on the floor. Take a few deep breaths to start and then, on an exhale, draw your pelvic floor muscles in and up (belly button towards your spine) as if you were trying to stop the flow of urine while peeing.
Hold your breath and the contraction for a couple of seconds, then inhale and release the pelvic floor muscles, letting your belly expand. Repeat for five reps.
4. Squats w/ Kegel:
Stand with your feet hip-width apart and take a few deep breaths. Exhale as you contract your pelvic floor muscles into a kegel and simultaneously bend at the knees, lowering your butt towards the floor. Keep your back in a straight posture, leaning slightly forward with your knees in line with your toes.
Focus on tightening your glutes as you raise back up to standing position (hold the kegel while going down and back up). At the top, release the kegel, take a couple of breaths, and then repeat for about 10 reps.
Pelvic floor lengthening exercises:
1. Happy Baby Pose:
This yoga stretch is great for opening your hips and stretching out your pelvic floor muscles anytime they feel tight. Lie on your back and bend your knees into your belly. Inhale, then grip the outsides of your feet with your hands.
Open your knees slightly wider than your torso, gently stretching your feet up towards your armpits (keeping your shins parallel to the floor). Deepen the stretch by pushing your feet deeper into your hands and pulling down through your fingers to create resistance. Hold for 1-2 minutes.
2. Seated Butterfly Stretch:
Sit on the floor with your back straight, shoulders down, and engage the muscles of your abdomen. Place the soles of your feet together in front of you with your knees open out to the sides (creating the “butterfly wings”).
Carefully and gently pull your heels towards you while simultaneously relaxing your knees towards the floor. To deepen the stretch, fold your torso slowly forwards over your legs, keeping your spine straight—but don’t overdo it. Breathe deeply and hold for about 30 seconds.
3. Figure 4 (Piriformis) Stretch:
Lie on your back with your feet flat on the floor. Cross your right ankle over your left knee, keeping your right foot flexed. Next, lift your left knee slowly towards your chest.
To deepen the stretch, interlace your fingers just below the crease of your left knee, gently pulling your knee in towards your chest. Hold for at least five breaths, then release and repeat on the other side.
4. Diaphragmatic Breathing:
Lie on your back on a flat surface or in bed, with your knees bent and your head supported. You can use a pillow, blanket, or bolster under your head and/or knees to get comfortable. Place one hand on your upper chest and the other just below your rib cage so you can feel your diaphragm move as you breathe.
Breathe in slowly through your nose so that your stomach moves out against your hand. When you exhale, tighten your stomach muscles, letting them fall inward as your belly button drops down towards the floor. Repeat for 3-5 minutes daily.
5. Deep Squat Stretch:
From standing, step your feet slightly wider than your hips. Squat down as deep as you can go, keeping your back flat and your hips centered over your ankles. Place your elbows on the insides of your knees and press your palms together, pushing your elbows into your inner thighs to create resistance. Keep your chest lifted, abdominal muscles engaged, and tailbone pointed down while breathing deeply for 30 seconds to one minute.
How do pelvic floor exercises help with urinary incontinence?
Pelvic floor exercises strengthen the muscles that support the pelvic organs and control urination. By improving muscle tone and control, these exercises can reduce urinary incontinence by helping to prevent leaks and improve bladder control. Consistency is key for optimal results. It can also help with chronic constipation.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2025 The Flex Company. All Rights Reserved.
- Wu, J. M., Vaughan, C. P., Goode, P. S., Redden, D. T., Burgio, K. L., Richter, H. E., & Markland, A. D. (2014). Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstetrics and gynecology, 123(1), 141–148. https://doi.org/10.1097/AOG.0000000000000057[↩][↩]
- Graber, B., & Kline-Graber, G. (1979). Female orgasm: role of pubococcygeus muscle. The Journal of Clinical Psychiatry, 40(8), 348-351. https://europepmc.org/article/med/468760[↩][↩]
- Lowenstein, L., Gruenwald, I., Gartman, I., & Vardi, Y. (2010). Can stronger pelvic muscle floor improve sexual function? International Urogynecology Journal, 21(5), 553-556. https://doi.org/10.1007/s00192-009-1077-5[↩]
- Mayo Clinic. (2020, April 23). Treating patients with pelvic floor dysfunction. https://www.mayoclinic.org/medical-professionals/physical-medicine-rehabilitation/news/treating-patients-with-pelvic-floor-dysfunction/mac-20431390[↩]
- What is pelvic floor physical therapy? (2018, September 21). ISSM. https://www.issm.info/sexual-health-qa/what-is-pelvic-floor-physical-therapy/[↩]
- Harvard Health Publishing. (2020, June 17). Pelvic physical therapy: Another potential treatment option. Harvard Health. https://www.health.harvard.edu/womens-health/pelvic-physical-therapy-another-potential-treatment-option[↩][↩][↩]
- Dale, R., & Stacey, B. (2016). Multimodal treatment of chronic pain. Medical Clinics of North America, 100(1), 55-64. https://doi.org/10.1016/j.mcna.2015.08.012[↩]
- Physiopedia. (n.d.). Myofascial pelvic pain. https://www.physio-pedia.com/Myofascial_Pelvic_Pain[↩]
- Cammu, H., & Van Nylen, M. (1995). Pelvic floor muscle exercises: 5 years later. Urology, 45(1), 113-117. https://doi.org/10.1016/s0090-4295(95)97180-7[↩]