Cervical cancer screening is important (and not that scary – we promise)
Every year, around 13,000 people in the US are diagnosed with cervical cancer, and 4,000 people die from it. Those are hard statistics, but that doesn’t mean you have to become one. Getting regular Pap test can tip you off to cervical changes long before they become a problem.
What is a Pap smear – and why is it called that?
Named after its inventor, Dr. Georgios Papanikolaou, a Pap smear (also referred to as a Pap test) is a test to find if any cells in your cervix have been affected by the Human Papillomavirus (HPV).
With over 200 strain variations, HPV is the most common STI in the world: More than half of the population is infected with it, and around 30 strains have been shown to eventually lead to cervical cancer if left untreated.
There’s lots of conflicting information about who needs to get Pap smears and how often. We are here with the latest information you need to maintain cervical health.
When to start & how often should you get a Pap Smear
Most people need to start getting Pap smears by age 21. HPV is a sexually transmitted disease–including via oral and anal sex, and possibly even kissing–so it’s time to start getting Pap smears once you have become sexually active.
Your doctor will tell you how often you need to get screened. According to the latest health guides and US standards, most people need a Pap test every 3-5 years, but your personal recommended frequency depends on several factors. Your age group, lifestyle, health history, and whether you smoke will influence your doctor’s recommendations, as will a weakened immune system or a medical history of irregular pap test results.

Can you get a Pap Smear on your period?
You can schedule a Pap smear with a family doctor or gynecologist, at a sexual health clinic, or at Planned Parenthood. Schedule it at a time when you do not expect to be on your period.
What to expect during a Pap smear
There’s no special preparation you need before your appointment, but to avoid obscuring test results, avoid sex and tampon use a day or two before. If you douche (which, according to most doctors, you shouldn’t EVER) avoid that before your appointment, as well.
The procedure is typically very quick and straightforward. It only takes a few minutes and should be relatively painless (you might feel a quick pinch-like sensation but you might not feel anything at all).
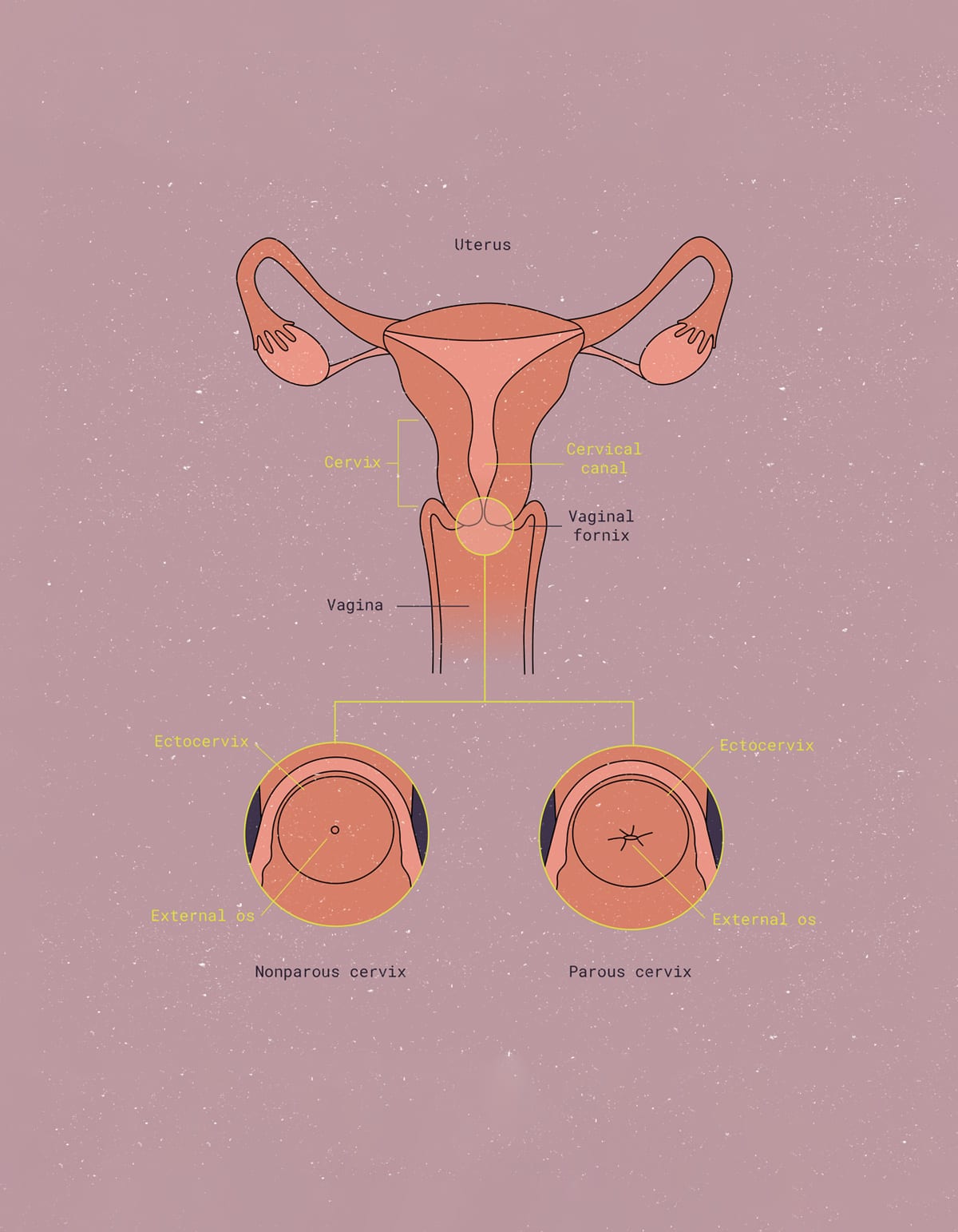
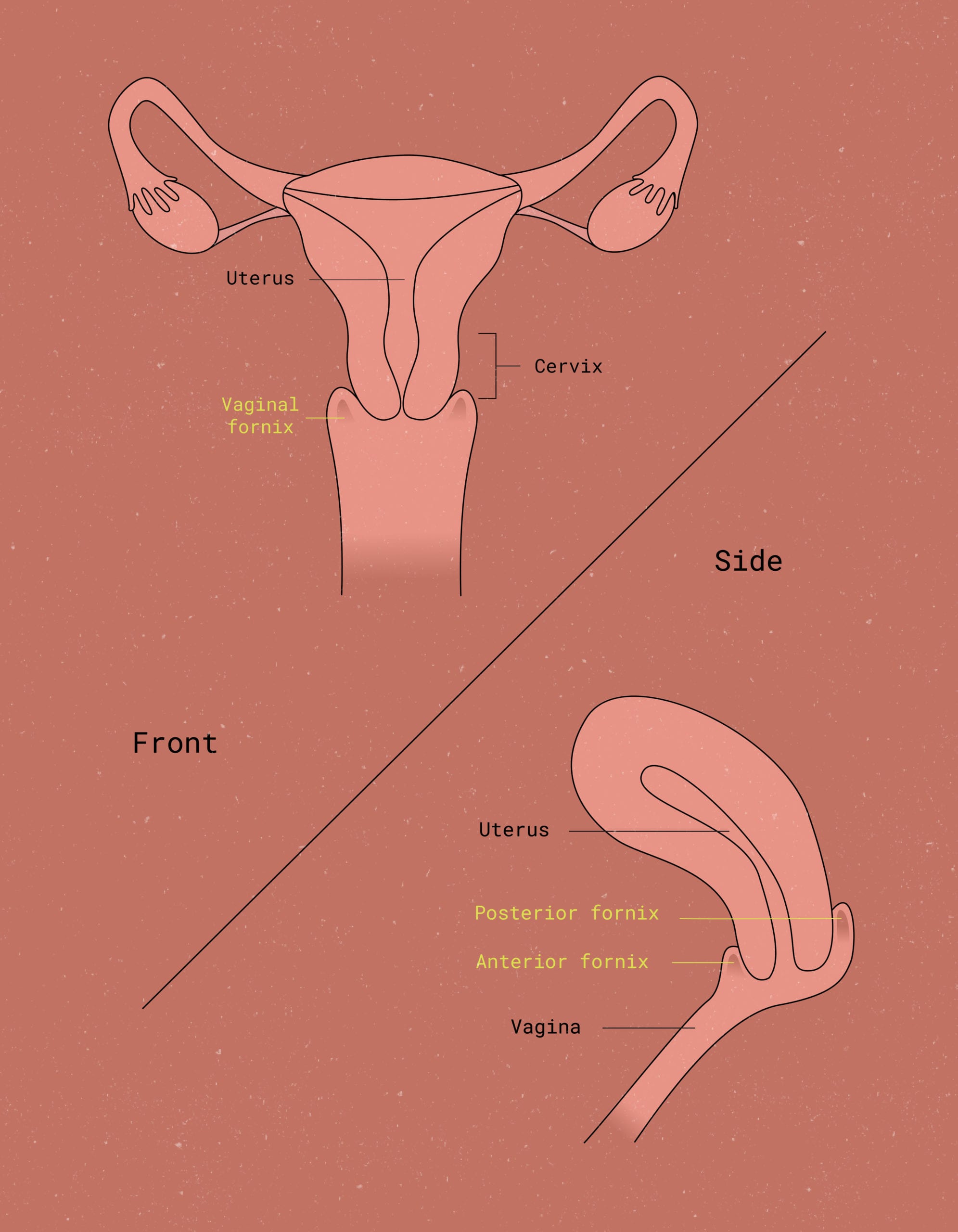
While you lay down on an exam table with your feet in the stirrups, a doctor or nurse inserts a metal or plastic speculum to widen the walls of your vagina, allowing access to the cervix (the narrow end of the uterus). They then take a tiny spatula or brush and collect cells from the surface of the cervix with a gentle swabbing action. That’s it.
Does a Pap Smear Hurt?
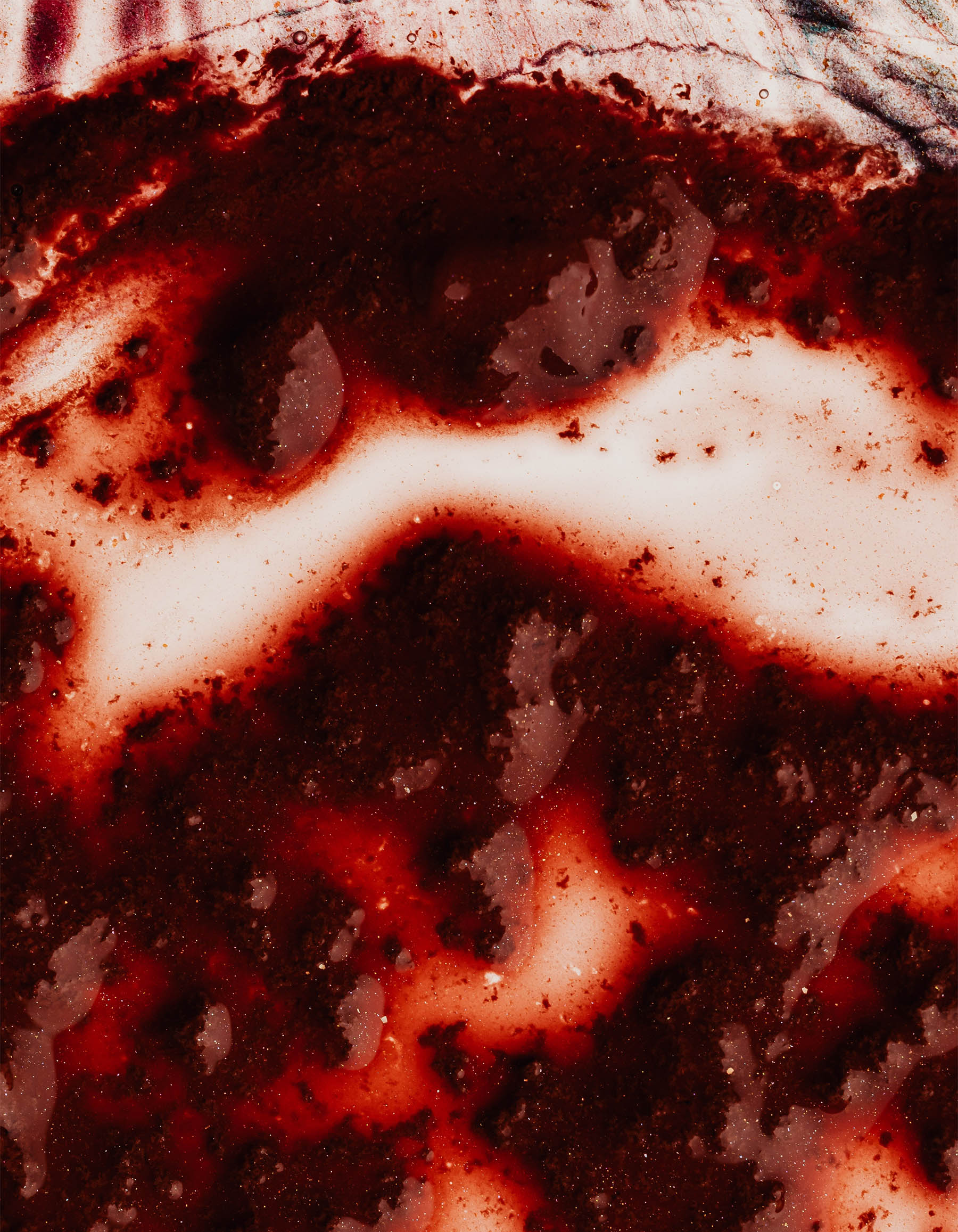
Some people experience slight discomfort from the speculum or a scratching feeling from the swab, but it’s momentary and nothing to stress out about. Slight bleeding after a Pap smear is common even if you’re in good health – this is mostly from the cervical scratch and should heal quickly.
If you do notice some spotting afterward, avoid putting anything in your vagina (such as a menstrual cup, menstrual disc, or tampon) to catch the bleeding. Your health care provider can give you a pad or you can bring one with you.
Getting your Pap Smear results
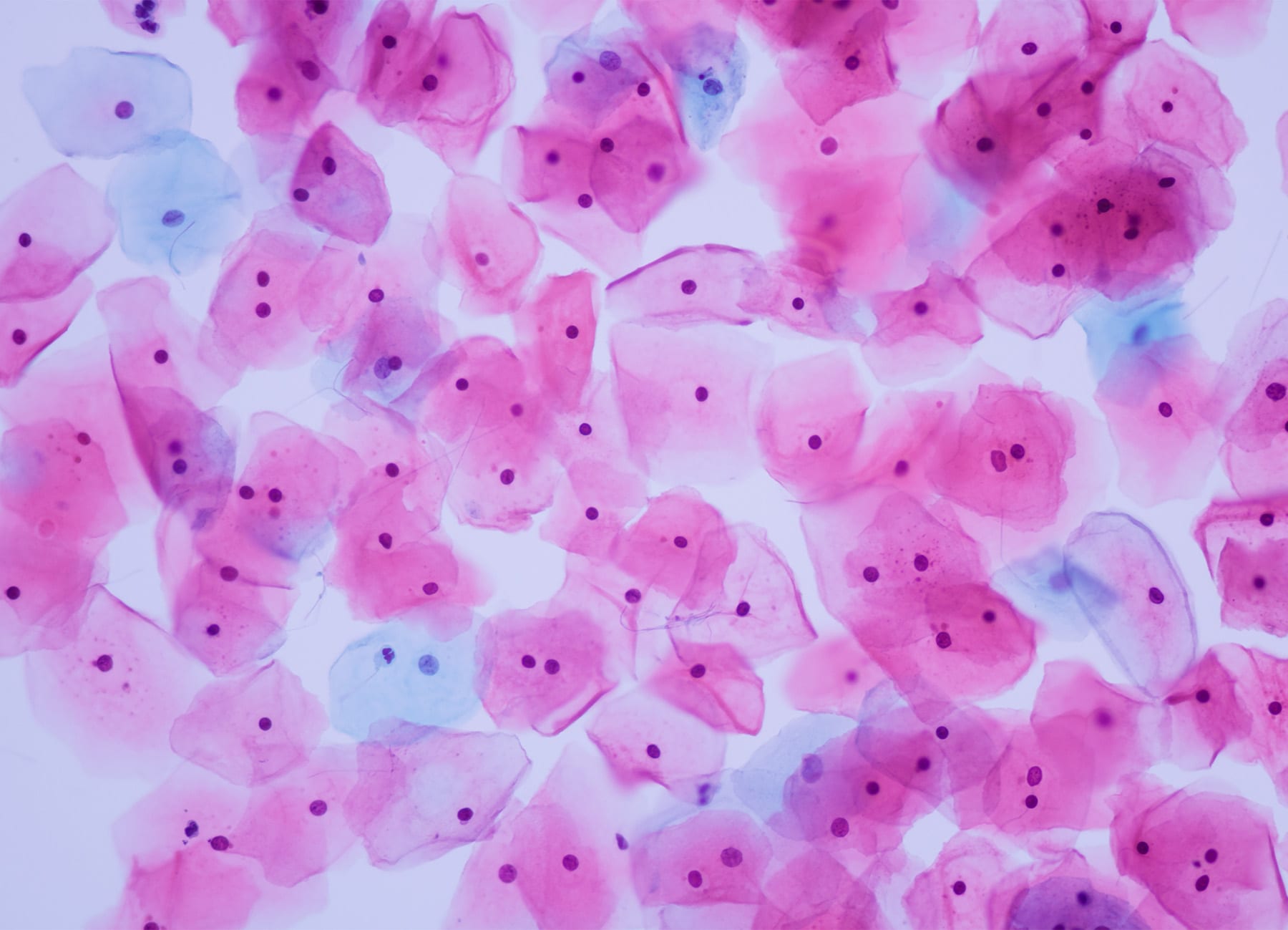
After you get a Pap smear, your doctor sends the cervical tissue sample cells to a lab for testing. The results will take anywhere from one to three weeks to arrive. You usually call your healthcare provider’s office to get the results, or they will call you. In some cases, you’ll get your results digitally via a patient portal.
Your test will have one of three outcomes:
- Normal: The cervical cells look normal, and you don’t need to do anything until your next regularly scheduled test.
- Abnormal: The sample of cells collected looks abnormal. This does not mean you have cancer. Depending on what the abnormal cell changes look like, your doctor will tell you what to do next. You may need to get another Pap smear immediately or within six months. If the cell changes look more serious, your doctor may recommend you get other cervical cancer screening tests, or further testing such as a colposcopy and/or a cervical biopsy.
- Unclear: Your doctor was not able to determine from the test if the cell sample looked normal or abnormal. They may order to repeat the test immediately, or in 6 months to a year.
Unclear or Abnormal Pap smear results
If your test results came back as anything other than normal, there could be a reason that has nothing to do with Human Papillomavirus (HPV) or cancer. Common factors affecting the results of a Pap Smear are:
- A yeast infection or other inflammation
- Benign (not cancerous) growths or cysts
- Changes in hormones from pregnancy or menopause
- Smoking
- Immune system problems such as diabetes, HIV, or other autoimmune diseases
Your doctor will discuss with you what next steps you should take after an unclear or abnormal test result.
Pap smear risks & considerations
As with any test that screens for disease or injury, there is a chance that a Pap smear will not detect cervical cell abnormalities that are there. Luckily, cervical cancer takes a relatively long time (10 to 20 years) to develop, so having a regular screen for cervical cancer increases your chances of detecting any abnormalities early on.
There is also a small chance that your results will come back abnormal even though there are no abnormal cervical cells. This is why your doctor or OB-GYN will recommend follow-ups for any abnormal pap test results.
Pap smears are not STI/STD tests
Pap smears are only designed to detect cervical cell changes that could indicate cervical cancer and potentially precancerous cells (intraepithelial lesions). They are not STD or STI tests and cannot detect viruses or diseases, including the HPV virus that causes cancer of the cervix, nor do they detect other cancers of the reproductive system, such as ovarian cancer.
However, a Pap smear and STD/ STI test can be done at the same time. Many providers recommend this or do it by default, especially when it comes to HPV testing. An HPV test checks your cells for the presence of a couple of high-risk strains of the HPV virus, but does not detect cancerous cells and is therefore not a replacement for a Pap smear.
Keep in mind that HPV infection is incredibly common and many strains clear up on their own within a couple of years. In addition, they can only be performed on people with female genitals. Your doctor may recommend an HPV test as a follow-up if you have a Pap smear result that comes back unclear or abnormal.
HPV tests can also be useful to let you know if you carry a high-risk strain, as your doctor may then recommend getting screening tests more often.

Lower your chances of cervical cancer
o lower your chances of cervical cancer, you can do the following:
Practice safer oral and penetrative sex.
This means using items such as dental dams and condoms and limiting consumption of substances that may impair judgment before sex. Safe sex is crucial in reducing your risk of contracting sexually transmitted infections, including the HPV virus.
Stop douching.
Douching removes the normal, healthy bacteria from your vagina that protect against infection, so avoiding it may also increase your protection against STDs/STIs. It is important to let your body maintain its natural cleaning process without interference from douching products.
Talk to your doctor about the HPV vaccine.
It protects against several of the most deadly strains. Also known by the brand name Gardasil 9, this HPV vaccine is a series of 2-3 shots that protect against several strains known to cause most cases of cancer and genital warts.
The HPV vaccine ensures that your body builds immunity against specific strains of the human papillomavirus, reducing your risk of developing cervical cancer in the future. By discussing this vaccine with your healthcare provider, you can make an informed decision to protect yourself from potential risks associated with HPV infections.

Get regular Pap smears.
Studies have shown that when detected via regular Pap smears, people who have cervical cancer have a 92% cure rate, versus 66% in those who discovered their cancer via other symptoms. A large majority of the people who die from cervical cancer were not following cervical cancer screening recommendations.
Regular screening is essential in detecting any abnormal changes in the cervix early on, allowing for timely intervention and treatment. By keeping up with regular Pap tests as recommended by your healthcare provider, you increase your chances of detecting any potential issues before they progress into something more serious. This simple screening test is a powerful tool in the prevention and early detection of cervical cancer, ultimately saving lives. Remember, your health is worth prioritizing.
Key Takeaways
There is no question about it: Pap Smears save lives.
Maintaining open communication with your doctor about any concerns or questions related to Pap smears, HPV tests, and preventive measures for cervical cancer is essential for your overall reproductive health. Regular screenings and following recommended guidelines can empower you to take proactive steps toward safeguarding your well-being.