What happens when Covid meets your period
Finally, nearly a year after the initial shelter-in-place and lockdowns went into effect, we are beginning to see a light at the end of a very, very, very long tunnel. Our bathrooms are fully stocked with TP, we’ve mastered the art of masking up one-handed (or not), and we’ve graduated from baking banana bread to binging Bridgerton (cue spoon scene here).
Though we may now be settling back into some semblance of a routine, it’s important that we take a step back and recognize just how broadly this pandemic has affected us – from our physical health to our mental and emotional wellbeing. And, for people with uteruses, the menstrual cycle is completely interwoven into each of those areas of wellness.
Like we’ve discussed in other posts, stress can have a huge effect on your period, from how you experience PMS to the length of your period itself. Given the stressors of a global pandemic on top of the many other things that happened this year (like, oh yeah, our election literally a couple months ago!), it makes sense that menstruation may have looked a little different in 2020.
But what about menstruators who actually contracted the virus? Will their fertility be impacted? Have their menstrual cycles changed? We still have a lot to learn about Covid-19’s long-term impact on overall health, but the CDC has officially recognized a few hallmarks of “long-haul” disease – including fatigue, joint pain, shortness of breath, and a stubborn cough.1 Nothing about periods, though (at least, not yet).
However: Between our colleagues here at Flex®, reports from our customers, and comments circulating around Facebook groups dedicated to Covid symptoms and experiences, we’ve seen tons of anecdotal evidence that Covid-19 can have an impact on the menstrual cycle. That it might lead to irregular cycles, increased period pain, or periods that are much heavier or lighter than usual.
And now, there’s even a tiny bit of research that’s begun to shed light on exactly what Covid’s impact on menstruation is, at least in the short term (keep reading!).
While we’re waiting for more official, peer-reviewed literature, we wanted to compile some of these Covid-meets-period stories and anecdotes into a blog post so that, if nothing else, people who are struggling with the long-term effects of the virus know they’re not alone. And, with any luck, we may even get the attention of some of the key players in the healthcare industry who can help us push for more funded research into the subject.
Important disclaimer before we dive in: The anecdotal information presented below is by no means meant to be taken as medical guidance. They’re stories that haven’t been scientifically or medically vetted – and as much as we’d like to think we’re experts on the menstrual cycle, we are neither medical researchers nor healthcare professionals. If you have a question or concern about your own health, PLEASE contact a licensed healthcare provider (not Dr. Google).
That said, let’s take a stab at the question of the day: Does Covid-19 affect the menstrual cycle? And if so, how – and why?
Covid & your period: Firsthand stories & experiences from the Flex Fam
You may have heard of “long Covid” or “Covid long-haulers,” terms referring to the potential long-term health effects experienced by a subset of people who’ve tested positive for the virus and, in some cases, even after they’ve recovered from the virus.
The CDC has a page on long Covid where they list out some of the reported symptoms, even broken out by organ system. As of the time that this post was written, the reproductive system is not listed explicitly on this page, although this is of course liable to change as more research emerges.
Given that all of our communities have been affected by this virus, The Fornix’s editorial team was interested in engaging with our online community to explore how some of us have been affected by Covid-19 and whether or not it’s led to weird (and in some cases, painful and frustrating) menstrual cycle changes.
In late January 2021, we put a call out on our social media pages asking our followers to share their stories with us if they were comfortable to do so. We got lots of incredible responses and we’re SO grateful to our wonderful community for being so open, willing to share, and supportive of one another.
It is so crucial to underscore that the following are anecdotes – personal stories from the awesome individuals who submitted them – and should not be construed as research, scientific commentary, or official guidance. Rather, this is a space to share, process, and reflect with one another in a digital (and socially distanced!) space.
So, without further ado:
Longer or heavier periods
Carly Glenn (@therealcarlyglenn) shared her experience with long Covid, which involved a loss of taste and smell that continued for months after her infection. She also notes that her period came back heavier and more painful post-Covid:
“I tested positive for Covid-19 in September 2020. It is now January 2021, and I still have no taste or smell [even though] my case was not severe. Emotionally, I started to experience changes, too. I felt frustration, more sadness and overall desperation to not be exhausted.
Also, not having your taste and smell as a PMSing woman is not fun. I knew I had cravings for things, but I didn’t know how to navigate what I wanted. Plus, I wouldn’t even be able to taste it anyways when it finally came down to making a decision.
Covid also came with extreme exhaustion, which completely paused my workout routines. When I first got my period after Covid, it was heavy and painful, and I was even more exhausted by it than usual. I found that drinking half of my body weight in water and adding some electrolytes to the mix was the perfect combination to feel decent.
Now, even without my taste or smell, my energy is back. Most days I eat an anti inflammatory diet so that when my period comes, my body is prepared. However, my body was not prepared for Covid, and I am still on the mend.”
Increased PMS and/or period pain
One Facebook user notes that, while fighting through Covid-19, she experienced heightened breast pain and more days of cramping leading up to her period (and at random times throughout the month):
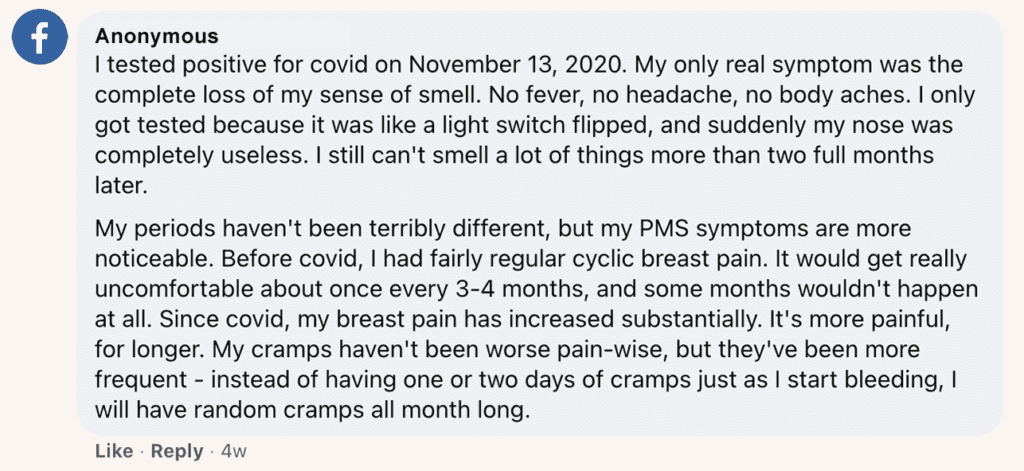
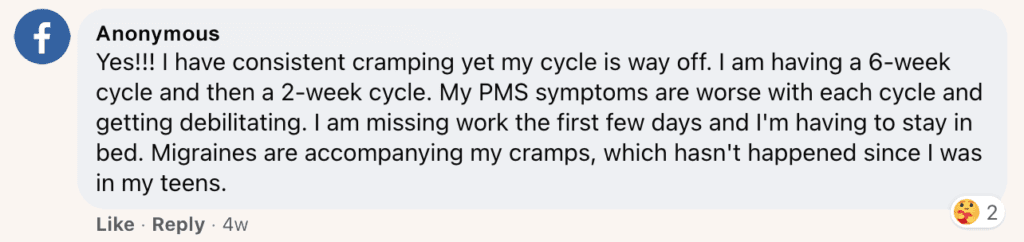
Another Facebook user has, since contracting Covid, noticed a significant increase in both PMS cramping and period pain:
Missed periods & irregular cycles
Margaret Baughman (@margbaughman) shared with us that she missed several periods after testing positive for Covid and still doesn’t know when to expect her next period:
“I started showing symptoms for Covid-19 at the end of March – less than two weeks after my city shut down – and had a mild case for about two weeks. Over the summer, my periods were definitely irregular, but I was fairly stressed with work and moved in with my partner, who also has a period, and thought it was maybe just that those things were making my cycle longer.
It jumped then to be two months between periods, and then when I got a period during the last week of September, I didn’t have another one until mid-January, almost four months late. I was so glad to know that I wasn’t at a risk of being pregnant because my partner doesn’t produce sperm, but as time went on, I definitely started to worry that something larger was wrong. My doctor tested me and didn’t find anything unusual, [but] going through those tests made me fairly worried.
I also experienced a lot of other seemingly-disconnected symptoms which made it unclear what the source of these things was. For about three months, I’ve been experiencing a lot of nausea and unhappiness in my stomach. When I finally got my period in January, it was the worst period I can remember having. Cramps, fatigue, more nausea, and such a heavy period.
I still have a bit of time before I expect a period again and have no idea whether I should actually expect it. 2020 is a different type of emotional stress than other times, but my day-to-day exertion and stress levels feel way lower than pre-Covid.”
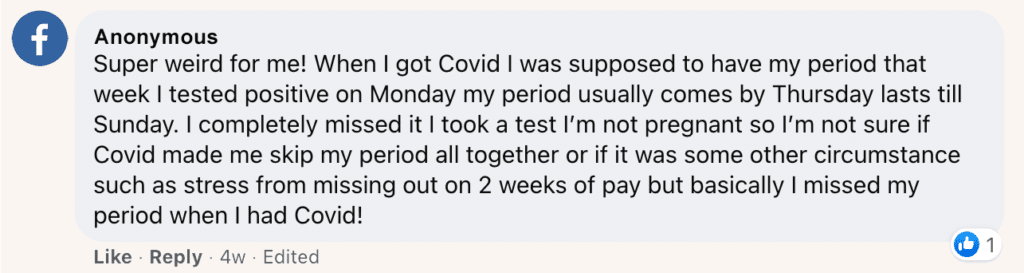
We heard from several others with accounts of missed periods or wildly irregular cycles:
Another user shares:
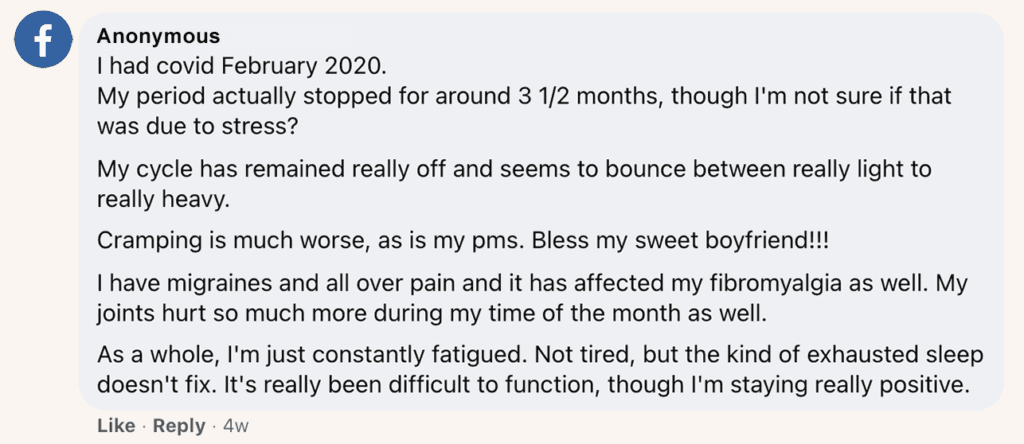
Other reported symptoms:
The most common shared experience among individuals who reached out to us who had been diagnosed with Covid-19 appears to be menstrual cycle irregularity – and this isn’t totally surprising. As one user shared on Facebook,
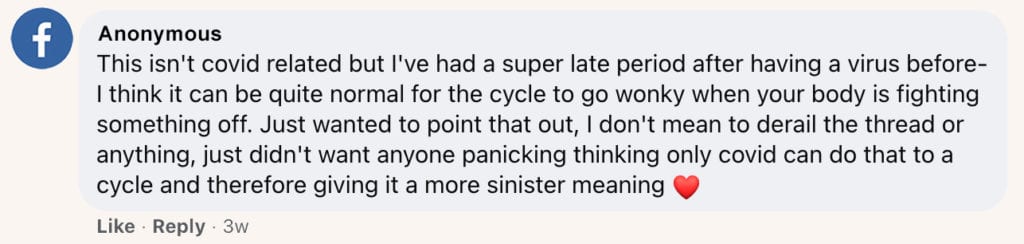
This note is 100% correct! Even before the pandemic, we’ve known that stress (both physical and emotional) can impact the menstrual cycle, leading to late or irregular cycles and, in some cases, more painful periods. However, we still need to conduct more research into specifically how viral stress on the body may influence your cycle during – or even after – a bout with illness.
For some menstruators, Covid made their period a little shorter and less painful. Maybe a silver lining for a lucky few? Lillian Boles (@lillian.boles) shared with us via email,
“My name is Lillian Boles and I’m 21 years old. I tested positive for Covid 19 on December 24 but took the test on December 23 and had been having symptoms for a couple of days.
My only symptoms were coughing and sneezing and body aches. My period started January 2 and lasted until January 4. It started on time but that was the shortest period I’ve ever had in my life.
My cycle has made some changes since having my daughter 22 months ago. I just finished my period and it was back to a normal 7 days. It’s usually 5 – 7 days long. My period in January was pretty painless. I normally take one Tylenol on day one for cramps but I didn’t take anything that time.
I have noticed that since I switched to the Flex Cup about 6 months ago, my cramps have been less painful and my cycles are sometimes 5 or 6 days when they used to always be 7 days. I love my Flex Cup and that it’s very comfortable and reusable!”
We appreciate the Flex Cup™ love! Hopefully, Flex has made things a little easier for those coping with Covid and a period at the same time.
Covid & pregnancy: Reproductive health experts weigh in
Before we get into what little research exists around Covid and periods, let’s recap a bit of good news: There’s been a decent amount of progress made in recent months re: the effect of Covid-19 (as well as Covid-19 vaccination) on pregnant individuals.
Earlier this month, the American College of Obstetricians and Gynecologists (ACOGACOG stands for the American College of Obstetricians and Gynecologists (a professional membership organization for obstetrician–gynecologists).), the American Society for Reproductive Medicine (ASRM) and the Society for Maternal-Fetal Medicine (SMFM) released a joint statement on guidance for pregnant persons and the vaccine.2
Here’s an excerpt from the statement:
“As experts in reproductive health, we continue to recommend that the vaccine be available to pregnant individuals. We also assure patients that there is no evidence that the vaccine can lead to loss of fertility. While fertility was not specifically studied in the clinical trials of the vaccine, no loss of fertility has been reported among trial participants or among the millions who have received the vaccines since their authorization, and no signs of infertility appeared in animal studies. Loss of fertility is scientifically unlikely.”
It is important to note that this is an ongoing conversation, and many professional organizations are continuing to revisit and reassess these questions as more information becomes available. Learn more via the link in the Tweet below from the CDC:
For a great compendium of information related to reproductive health and the novel coronavirus, give this practice advisory from ACOGACOG stands for the American College of Obstetricians and Gynecologists (a professional membership organization for obstetrician–gynecologists). a read. This source will continue to be updated as more information becomes available; it goes into more detail around the reasoning and data behind ACOG’s decision.
Covid & your period: What the science says
Although it’s helpful and impactful to see some official guidance around pregnancy and Covid-19, we’re still left with a pretty huge knowledge gap. Specifically, knowledge pertaining to people with uteruses on either end of the spectrum, from menstruators to pre- and post-menopausal individuals.
Excitingly, one recent study performed in Shanghai (published January 2021) DOES address this question of ours – i.e. how Covid-19 impacts the menstrual cycle.
The researchers did so by collecting data on reproductive hormones, menstrual cycle characteristics, and ovarian reserve from women with confirmed SARS-CoV-2 infection.3 This study included 237 patients in total, of which 177 had menstrual data available. FYI, all of the women in this study were of child-bearing age.
The findings showed that in this population, 25% of women with Covid had changes in their menstrual cycle. In all, 20% had a decrease in menstrual cycle volume (a.k.a. a lighter period) whereas 5% had an increase in volume (a heavier period). There was no statistically significant difference in menstrual cycle volume identified between the mild and severely ill sub-populations.
However, things looked a little different when it came to menstrual cycle length. In short, severely ill women had longer menstrual cycles compared to their counterparts, with 34% of severely ill patients having a cycle of longer than 37 days. For a quick refresher on what this all means in context, check out our first Re: Your Cycle post that outlines the stages of the menstrual cycle.
Menstrual cycle characteristics were also compared pre- and post- Covid infection. This study did not find any statistically significant difference in menstrual cycle length for these patients throughout the six months of follow-up.
“25% of women with Covid had changes in their menstrual cycle. In all, 20% had a decrease in menstrual cycle volume (a.k.a. a lighter period) whereas 5% had an increase in volume (a heavier period).”
But, when these patients were followed-up individually after discharge, eight women who had experienced decreased menstrual volume had not returned to normal, and one patient’s menstrual cycle length had not yet normalized, either. This goes to show that statistical significance doesn’t always translate to individual experience.
If you’re interested in learning more about this study, we’d urge you to go to the source itself, again hyperlinked here. Pro tip: During the Covid pandemic, many online publishers are making literature about the virus free to read to encourage public education.
Also, take a look at this research from the British Journal of Sports Medicine:
Experiencing symptoms? Reach out to your OB-GYN
Soapbox moment here: If you are ever experiencing symptoms with your period that are new for you, like pelvic pain, painful periods, spotting or bleeding outside of your cycle, migraines, nausea/vomiting, etc., don’t hesitate: Reach out to your primary care provider or your OB/GYN as soon as possible.
If you think that you may have had a Covid exposure, or if you ever tested positive for Covid, make sure to bring it up during your appointment: It could be helpful information for your provider to reference when determining the best course of action for diagnosis and care.
Once more, we would like to reiterate that we are still in the early stages of understanding the effects of Covid on the human body, and that the stories presented here are just that: Stories, shared by individuals, colored by their own unique experiences and health history. For medical information, guidance, and resources, reach out to a licensed healthcare provider.
Important information & additional resources
If you’ve tested positive for Covid-19 or have been experiencing symptoms such as fever, chills, cough, loss of sense of taste or smell, shortness of breath or difficulty breathing, sore throat, or intense fatigue, get in touch with a healthcare provider ASAP and make sure to follow official CDC guidance on how to proceed.
When searching the Internet for information and resources regarding Covid-19, make sure to check your sources. Trusted sources like the CDC and WHO are your best bet for accurate, reliable, and up-to-date information. Here are a few important links:
- The CDC Page on Covid-19
- The WHO Page on Covid-19
- The PAHO Page on Covid-19
- The American Public Health Association Page on Covid-19, especially for advocacy initiatives around health equity.
- The BMJ on Long Covid, including a summary from researchers in the field as well as a video webinar.
- FDA Website on Vaccine Updates
- HHS Website on Vaccine Updates, a bit more user-friendly to read
- NYT Coronavirus Vaccine Tracker, has graphics if you are a visual learner as well as recent news
- HHS Resource to Find Testing Near You, enter your zip code here to find a community-based testing site in your city/state
- The ACOG Page on Covid-19, a resource from the medical society of OB/GYNs on reproductive health-specific Covid updates
How to advocate for menstrual cycle research
Patient advocacy groups and medical societies alike are taking up this gauntlet of advocating for more research on people with uteruses – but you have a role to play, too.
Here are a couple of actionable to-dos if you’re interested in becoming engaged with this work:
- Connect with your local Planned Parenthood chapter. This org is often at the forefront of reproductive healthcare advocacy, and there may be a volunteer opportunity near you (virtual, of course).
- Call or email your local representative and urge them to advocate for the support of reproductive health research at the local and federal levels.
- Join the conversation on social media: From IG to Twitter and even Slack, there’s a virtual community somewhere out there that you can learn from and contribute to.
Covid & your period: Final thoughts
During this difficult time, community is more important than ever. If you’ve had or recently recovered from Covid-19, we hope that this post has given you a bit of solace.
If you’re dealing with difficult, long-term symptoms of the virus, unpredictable menstrual cycles, or unrelenting pain and fatigue, know that you’re not alone.
We also hope that this post has perhaps answered a question or two you’ve had about Covid and your period. If it’s brought up more questions than answers, that’s perfectly fine, too! Think of this as a jumping-off point for you to learn more about Covid-19 and the menstrual cycle, especially as more research continues to emerge on a daily basis.
Here at Flex, we’re committed to fighting period stigma and opening up the conversation around menstruation – even and especially during a pandemic. If you have any feedback about this post, or if you’ve come across a new study or piece of research that you’d like to see us spotlight, feel free to reach out to us at thefornix@flexfits.com.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2021 The Flex Company. All Rights Reserved.
- Centers for Disease Control and Prevention. (2020, September 17). Coronavirus disease 2019 (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html[↩]
- ASRM. (2021, February 5). ASRM, ACOGACOG stands for the American College of Obstetricians and Gynecologists (a professional membership organization for obstetrician–gynecologists). and SMFM Issue Joint Statement: Medical Experts Continue to Assert that COVID Vaccines Do Not Impact Fertility. Retrieved February 11, 2021, from https://www.asrm.org/covid-vaccine-and-fertility[↩]
- Li, K., Chen, G., Hou, H., Liao, Q., Chen, J., Bai, H., Lee, S., Wang, C., Li, H., Cheng, L., & Ai, J. (2021). Analysis of sex hormones and menstruation in COVID-19 women of child-bearing age. Reproductive Biomedicine Online, 42(1), 260–267. https://doi.org/10.1016/j.rbmo.2020.09.020[↩]