Pelvic Inflammatory Disease: Causes, symptoms & treatment
Here’s what to know about PID
May is Pelvic Pain Awareness Month—and this year, we’re creating space to discuss a reproductive health condition that’s still a bit of a medical mystery: Pelvic Inflammatory Disease (PID).
Pelvic Inflammatory Disease is pretty common, affecting over a million people AFABAFAB stands for “assigned female at birth.” in the U.S. per year1 It’s one of the conditions that your gynecologist may screen for at your next annual visit, usually by asking you a series of questions—but there isn’t one set way to diagnose it. In fact, the diagnostic criteria are mainly based on symptoms that you report to your provider (as opposed to the lab tests used to diagnose STIs, for instance).
One of the mainstays of Pelvic Inflammatory Disease is pelvic pain. We’re talking more than the average set of cramps that come along with your period once a month: PID pain is mild to severe and can be felt from your pelvic region all the way up to your upper abdomen (usually on the right side, but it can be felt on both sides, too). This region may be dull, achy, stabbing, or bruise-like, and the area may be tender to the touch.
Pelvic pain associated with PID also usually comes with other signs and symptoms, which we’ll discuss momentarily. The name of the game today is to understand what exactly it is, the causes of PID, and potential treatments.
What is PID – and is it serious?
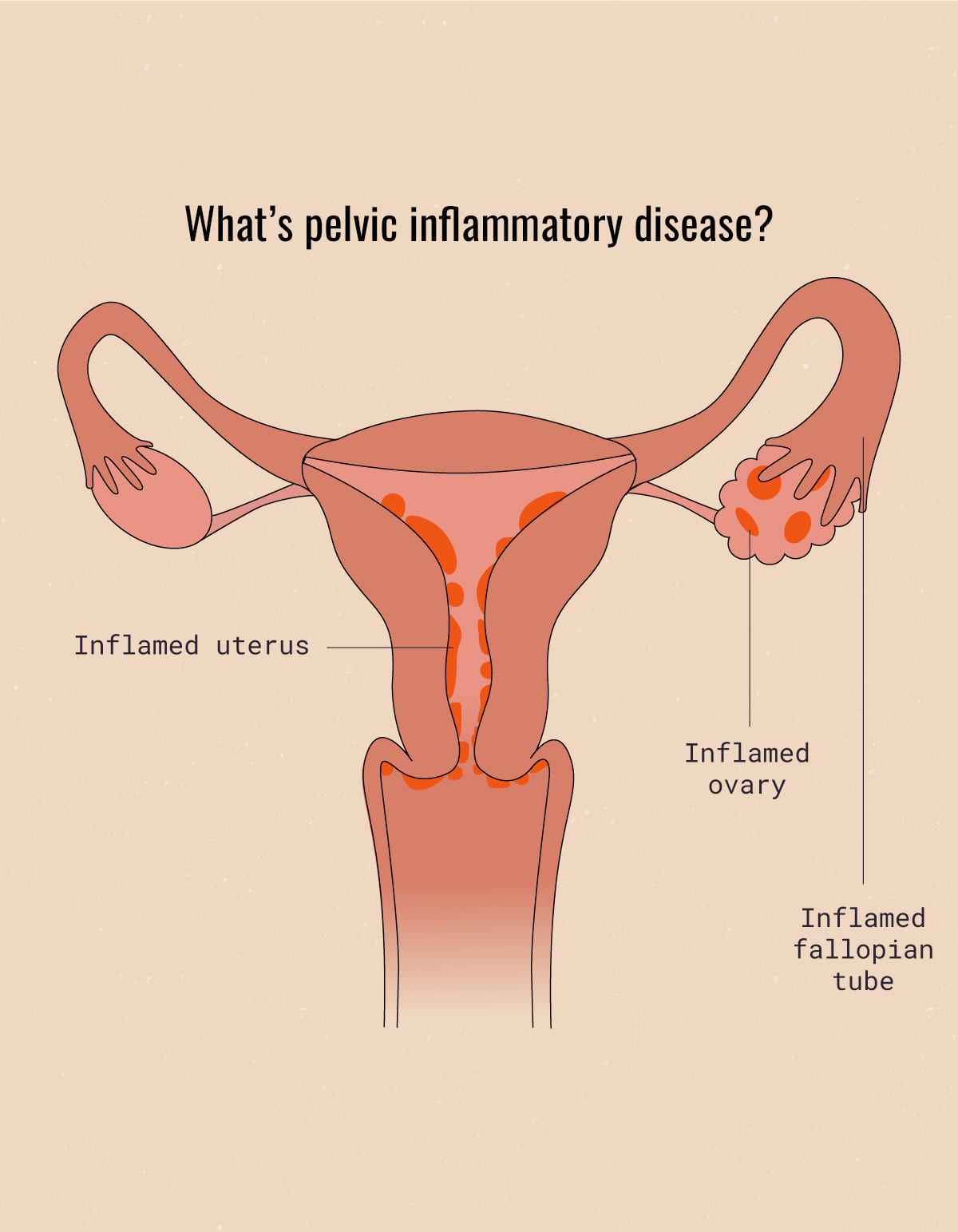
Pelvic Inflammatory Disease is an infection of the female reproductive organs. It’s also both, a diagnosis and a set of symptoms that are thought to encompass it (more on those signs and symptoms later). The basic idea around PID is that certain types of bacteria (bad bacteria) enter through the vagina and move upwards into the cervix, then into the uterus, ovaries, and/or the fallopian tubes.
Those last three are core parts of the reproductive system and, as such, they’re super sensitive to infection or inflammation. Bacteria that successfully invades the reproductive system can cause local inflammatory reactions, even leading to things like the formation of abscesses: an abscess is a collection of pus and infective material that cause severe pain and damage to the surrounding tissues.
In other words: Very, very bad.
Pelvic Inflammatory Disease & STIs: Is there a connection?
In many cases, Pelvic Inflammatory Disease is the end result of an untreated vaginal infection.2
The most common ones that can lead to PID are:
- Gonorrhea
- Chlamydia
- Mycoplasma Genitalium
- Bacterial vaginosis (BV)
To review, gonorrhea and chlamydia are STIs, meaning that they are spread via unprotected sex. Gonorrhea and chlamydia are most commonly found in the throat, rectum, urethra, and cervix. FYI, sexual contact means any form of sexual contact—including oral, vaginal, and anal sex.
Not only can PID be extremely painful for anywhere from days to weeks, but it also can have a long-term impact on your health and reproductive abilities. Left untreated, cases of PID can lead to chronic pelvic pain, ectopic pregnancy, or even infertility. It’s estimated that 1 in 10 AFABAFAB stands for “assigned female at birth.” with Pelvic Inflammatory Disease will eventually become infertile.

Those stats sound scary, but we’re not here to freak you out: What’s most important is that you know what PID looks and feels like so you feel empowered to reach out to a health care provider if you think something might be wrong. And thankfully, PID is treatable, especially when caught early (more on that below).
What causes PID?
Like we mentioned earlier, PID is caused by bad bacteria that get past the acidic vaginal canal (your repro system’s first line of defense) and make their way into the reproductive system—through your cervix, into your uterus, and potentially all the way up to your fallopian tubes and ovaries.
This type of bacteria most often belongs to STIs like gonorrhea and chlamydia. However, other bacterial infections (like bacterial vaginosis) can also lead to PID.
Who’s at risk for Pelvic Inflammatory Disease?
Technically speaking, anyone with a vagina can get Pelvic Inflammatory Disease. There are, however, a few factors that put certain people at a higher risk of PID:
- Being sexually active
- Having multiple sex partners
- Having a sex partner who has multiple other partners
- Having been diagnosed with PID in the past
- Having an untreated or undiagnosed STI
- Intrauterine Device (IUD) users (Note: This risk is typically related to the insertion of an intrauterine device and is higher within the first three weeks after the IUD is placed…more data pending.)
- Douching (Note: Douching often gets rid of the “good” bacteria and, in worst-case scenarios, can actually push the “bad” bacteria up there! For this reason, douching isn’t recommended by ACOGACOG stands for the American College of Obstetricians and Gynecologists (a professional membership organization for obstetrician–gynecologists).. Vaginas are self-cleaning, but if you just want to wash your labia, try using a gynecologist-recommended cleanser and rinse thoroughly with warm water. Just make sure not to put any soap INSIDE!
Keep in mind that you can get Pelvic Inflammatory Disease without being sexually active— severe cases of bacterial vaginosis, for instance, can lead to PID. So, no matter what your sex life is like, always talk to a healthcare provider if you notice unusual signs that might resemble symptoms of pelvic inflammatory disease, especially the ones outlined below.
Symptoms of Pelvic inflammatory disease
The symptoms of PID can vary from one person to another. In general, PID symptoms include:
- Pain in the pelvic area, potentially extending all the way from the upper stomach to the lower abdomen/pelvis
- Unusual vaginal discharge
- Vaginal odor that is fishy or foul-smelling
- Painful urination
- Abnormal uterine bleeding (i.e. spotting in between periods, bleeding after sex)
- Flu-like symptoms such as fever, chills, nausea, or vomiting
- Pain with sex
Out of all possible PID symptoms, pelvic pain is generally the most common. If you experience severe symptoms, such as severe pelvic pain, high fever, vomiting, or fainting spells, seek immediate medical attention or go to the emergency room immediately, as these could indicate a more serious complication of PID such as an abscess or sepsis.
PID Treatment: Early Diagnosis and Treatment Key to Preventing Long-Term Complications
Pelvic Inflammatory Disease treatment mostly focuses on addressing the underlying infection that caused it. For most infections, including Sexually Transmitted Infections STI, this is done via antibiotic treatment. However, if Pelvic Inflammatory Disease has progressed to later stages or if there are any abscesses or scar tissue, a more invasive treatment may be required.
If you experience pelvic pain along with a high fever, nausea, vomiting, fainting, or loss of consciousness, seek immediate medical attention. Contact a healthcare professional if you have any concerns about your health.
Something else that often is forgotten with Pelvic Inflammatory Disease? It might be uncomfortable, but you have to treat it like an STI—meaning, you should inform any sexual partners who might be at risk. While it might feel like the worst possible conversation to have, all parties involved will be grateful you did it in the long run.

PID Prevention and Additional Resources: What You Need to Know
One mainstay of PID prevention is practicing safe sex habits. Use a barrier method of birth control (like condoms), get tested frequently (especially before initiating sexual contact with a new partner), and don’t be scared to initiate that awkward conversation with partners about their sexual history—both past and current. STI prevention will also prevent Pelvic Inflammatory Disease.
STIs are the most common cause of PID, but not the only cause. Various infections can lead to PID. To prevent them, please avoid douching. Everyone in the medical community agrees that it only causes trouble and can lead to serious problems and long-term complications.
If you’re feeling any weird symptoms, like pain or burning when you pee, spotting blood when not on your menstrual period, or lower abdominal pain, swelling, or discomfort in your pelvic organs region, speak to a licensed healthcare provider. In the interim, click here for a short and sweet factsheet from the Centers for Disease Control and Prevention CDC.
PID: Key takeaways for a healthy life
PID stands for Pelvic Inflammatory Disease. It’s a set of signs and symptoms that are the result of bacteria spreading up into the female reproductive tract. The most common cause of PID is an untreated STI, but it can also be caused by other, not-necessarily-sexually-transmitted infections like bacterial vaginosis (BV).
Pelvic pain is one of the main symptoms of PID—but it can also involve painful urination, unusual discharge or odor, spotting, dyspareunia, and flu-like symptoms. The main way to treat PID is by treating the underlying infection and preventing further scarring or disease in the area.
One in ten people diagnosed with Pelvic Inflammatory Disease will go on to be infertile. To prevent PID, practice safe sex by using condoms and having open discussions with partners. Avoid douching and consult a healthcare provider for more information.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2025 The Flex Company. All Rights Reserved.
- ACOGACOG stands for the American College of Obstetricians and Gynecologists (a professional membership organization for obstetrician–gynecologists).. (2019, August). Pelvic inflammatory disease (PID). Retrieved April 19, 2021, from https://www.acog.org/womens-health/faqs/pelvic-inflammatory-disease[↩]
- CDC. (2020, November 19). Pelvic inflammatory disease – CDC Fact Sheet. Retrieved April 19, 2021, from https://www.cdc.gov/std/pid/stdfact-pid.htm[↩]