Understanding your fertility
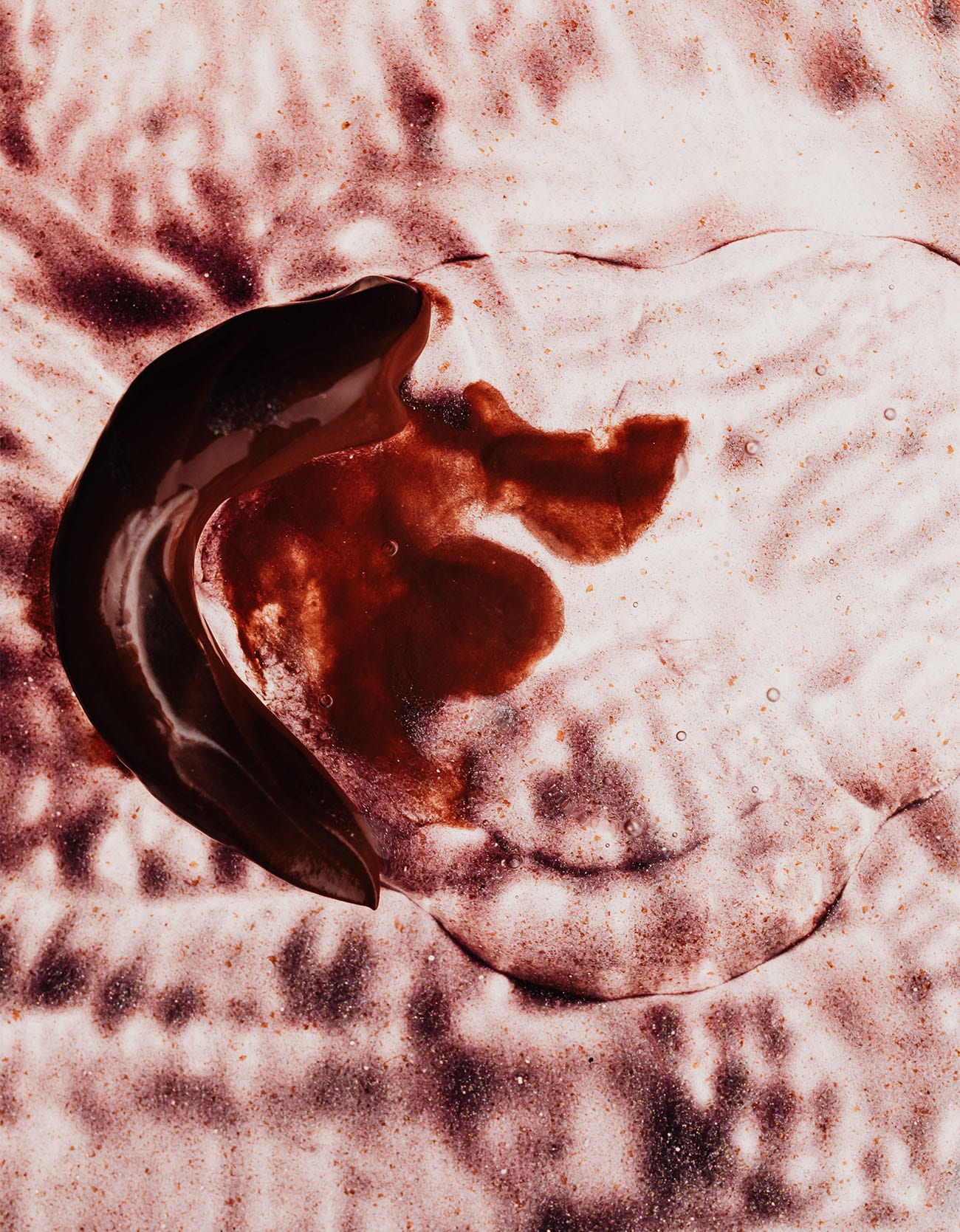
It’s about more than just pregnancy—an at-home fertility testing kit can help you learn more about your body, your period, and your overall health.
When you hear the word fertility, you may think of a clinic, In Vitro Fertilization (IVF) treatments, or babies. If these things aren’t on your radar, you might not be interested in thinking about it all that much more. But the reality is, fertility is about more than just your chances of pregnancy.
From how many eggs you have now to when you might hit menopause, insights about your hormone production, ovulation patterns and menstrual cycle can also tell you about your current health (if your hormone levels are high or low) and what may lie ahead in your future.
As someone living with a painful, genetically inherited condition, I have some serious thinking to do before I make the decision to carry a pregnancy or explore an alternative. As a 30-year-old woman, I also know that I don’t have infinite time to explore all of my options.


With Modern Fertility’s at-home testing and (most importantly) in-depth resources to help you understand what your test results mean, you can not only plan ahead but also learn more about your body in the present.
While an at-home test won’t provide a diagnosis of specific medical conditions (such as endometriosis, Pelvic Inflammatory Disease or Polycystic Ovary Syndrome PCOS), or give you an infertility diagnosis, it does give you important information about your reproductive health that you can take with you to your doctor.
How are hormonal changes and fertility related?
We think of hormonal changes as something that happens later in life due to menopause, but there’s more to it than that– hormones are responsible for much more than just reproduction. In fact, they are the messengers that tell our body’s systems how to function.
If there is an imbalance in your hormones or if you have a hormonal disorder, it might be the root cause of experiences like fatigue, sleep disturbances, ovulation disorders, dysmenorrhea (painful periods), and a myriad of other things. I’m always in favor of learning the cause of any discomfort in your body— even if it’s just the crucial step of ruling something out as a possible cause.
The pituitary gland plays a central role in regulating hormones related to fertility. It releases key hormones like luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which are essential for ovulation and the overall menstrual cycle. Any disruption in the pituitary gland’s function can lead to irregular cycles, making it vital to understand its influence on your reproductive health. Moreover, factors such as stress, diet, and lifestyle choices can further impact hormonal balance. Stress, for instance, has been shown to elevate cortisol levels, which can inhibit the production of reproductive hormones, leading to issues with ovulation.


Speaking of discomfort, fertility awareness can often be a sensitive topic to explore, which is why I love Modern Fertility’s approach. Every step of the process feels thoughtful and kind, like the bedside manner of a really good doctor.
There is also a fertility nurse available to answer any questions that you may have about your specific results. If that’s not enough, there’s the opportunity to join an online group of other Modern Fertility users, so you can feel fully supported in this process.
What causes female fertility problems?
Female infertility can arise from various factors. Some possible causes of infertility include hormonal imbalances, age-related decline in egg quality, physical and emotional stress,health conditions such as polycystic ovary syndrome (PCOS), cystic fibrosis, endometriosis, and other dysfunctions or issues of the female reproductive system. Lifestyle factors such as obesity, low body weight, smoking, and excessive alcohol consumption not only can increase your risk of miscarriage, but they can also result in a higher risk of infertility.
Environmental factors also play a role, including exposure to toxins, pollutants, and endocrine disruptors that can interfere with reproductive hormone balance and reproductive health. Understanding these variables is crucial, as knowledge empowers individuals to make informed decisions about their fertility journey. Moreover, the emotional and psychological aspects of fertility cannot be overlooked. Anxiety and depression can exacerbate physical symptoms and contribute to a cycle of stress that further impairs reproductive health. This interconnectedness highlights the importance of a holistic approach to fertility, one that acknowledges both the physical body and the mind.
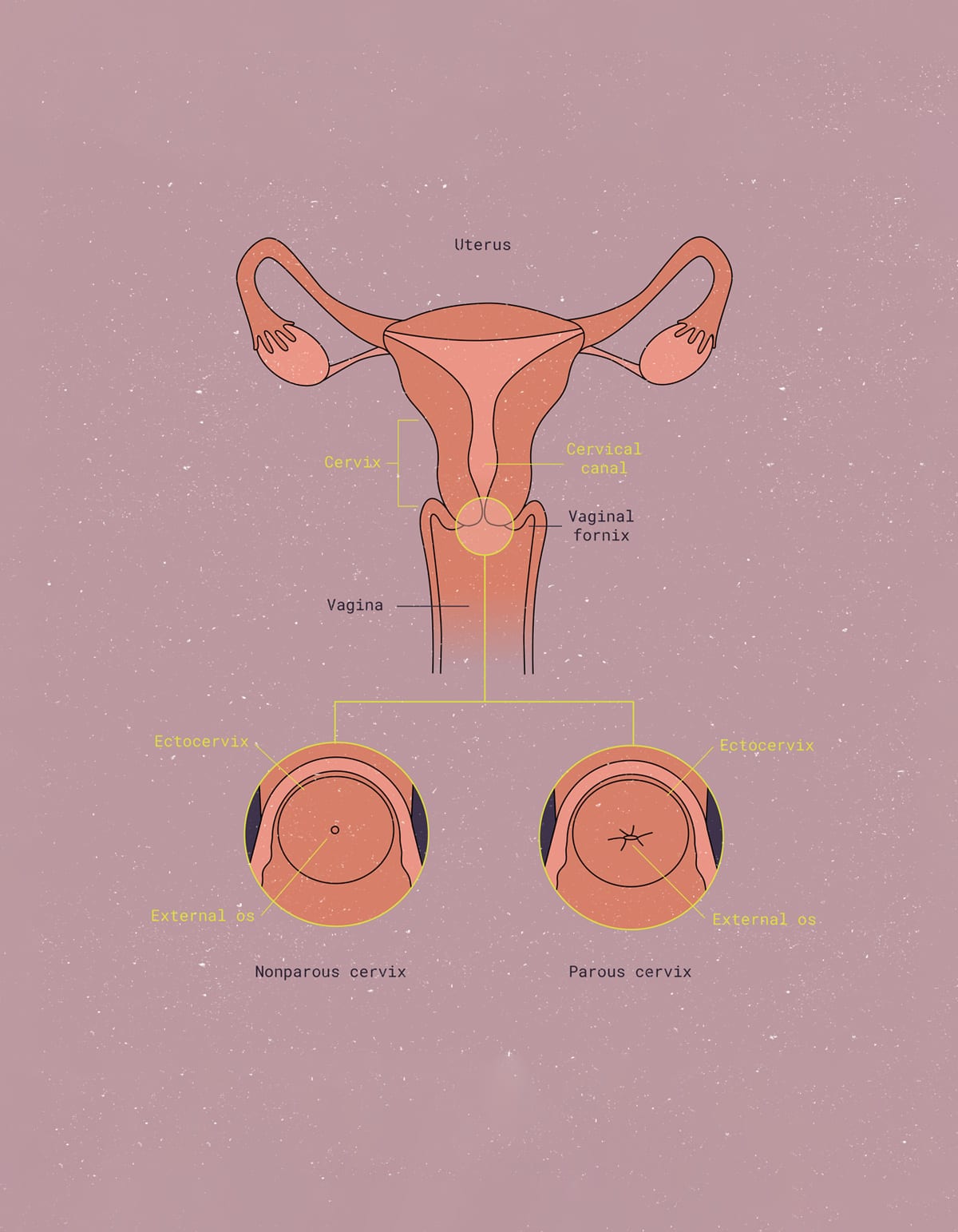
What are the most common causes of infertility in people with uteruses?
The most common cause of female fertility problems is ovulatory disorders, which account for a significant percentage of infertility cases. Conditions such as irregular periods and menstrual cycles or anovulation can prevent the release of eggs, making conception challenging. Hormonal imbalances, particularly involving estrogen and progesterone, can disrupt the normal ovulation process. Another prevalent issue involves structural problems within the reproductive system. Conditions like uterine fibroids, polyps, or blockages in the fallopian tubes can physically obstruct the path to fertilization or implantation. These anatomical challenges may often be addressed with medical intervention or surgical procedures.
It’s a good idea to approach fertility with both knowledge and compassion. Understanding the factors at play can empower women to make informed choices, whether they’re aiming for conception or simply seeking to understand their bodies better.
Regular check-ups and open conversations with healthcare providers are crucial steps in this journey. Beyond medical concerns, emotional support plays an essential role. Many women experience feelings of isolation or anxiety when facing fertility challenges. This is where fertility care services, community platforms and support groups can offer solace, providing a space to share experiences, advice, and encouragement. Furthermore, adopting a healthy lifestyle can enhance overall well-being and potentially improve fertility outcomes.
Types of infertility in women
There are two types of infertility: primary and secondary. Primary infertility refers to individuals or couples who have never conceived after a year of unprotected intercourse. This can stem from various factors, including age, genetic issues, or the aforementioned ovulatory disorders. Secondary infertility, on the other hand, affects those who have previously conceived but are struggling to achieve another pregnancy. This may occur for reasons such as changes in health status since the last pregnancy, age-related decline in fertility, or complications from previous births. Understanding these distinctions is vital for tailoring a suitable approach to treatment.
It’s not always on the female side of things
Infertility is not always just a female issue. In fact, male factors contribute to nearly half of all infertility cases. Some common causes of male infertility include erectile dysfunction, spem production issues such as low sperm count or poor sperm quality in term of motility. Additionally, structural issues can also impede conception just as much as female reproductive health problems.
It is essential for couples facing fertility challenges to seek a fertility specialist and undergo comprehensive evaluations together, as a holistic approach allows for a more accurate diagnosis and effective treatment options for infertile couples. In the realm of reproductive medicine, both female and male fertility treatment avenues vary widely, ranging from lifestyle changes and medication to assisted reproductive technologies like in vitro fertilization (IVF) or artificial insemination.


Evaluating your options: What treatment options are available
Depending on the cause of infertility, a variety of treatment options are available to assist individuals and couples in their journey toward conception. For those with hormonal imbalances, a reproductive endocrinologist can evaluate hormone levels and recommend therapies such as hormone replacement or medications to stimulate ovulation. For women facing structural issues, surgical options may include the removal of fibroids or polyps, or procedures to clear blockages in the fallopian tubes.
In cases where these interventions are insufficient, assisted reproductive technologies (ART) offer hope. Intrauterine insemination (IUI) can be an option for couples with less severe fertility issues, while in vitro fertilization (IVF) provides a more intensive approach by allowing for mature egg retrieval and fertilization outside the body before implantation.
Key Takeaways: Knowledge is Power
The bottom line? It can be scary to think about your fertility and hormones, but we’re lucky to have tools like Modern Fertility to help alleviate some of that fear. Knowledge is power, and learning more about your body is an act of self-empowerment.
When it comes to understanding our bodies, particularly in the realm of fertility, having access to reliable information is crucial. Hormones are intricately linked not only to reproduction but also to overall well-being. Their roles extend far beyond what we typically recognize, influencing everything from mood swings to fluctuations in weight. Modern Fertility’s user-centric approach demystifies this complex topic. With a focus on education and compassion, they provide resources that empower individuals to take charge of their reproductive health. The availability of a dedicated fertility nurse for personalized inquiries adds an essential layer of support, ensuring no question goes unanswered.
Health information seekers often turn to reliable sources to understand the various factors influencing fertility, including lifestyle choices, nutrition, and medical interventions.
Understanding your menstrual cycle and tracking ovulation can also significantly improve your chance of pregnancy (if you’re trying to conceive), as timing intercourse around this fertile window is crucial for conception.
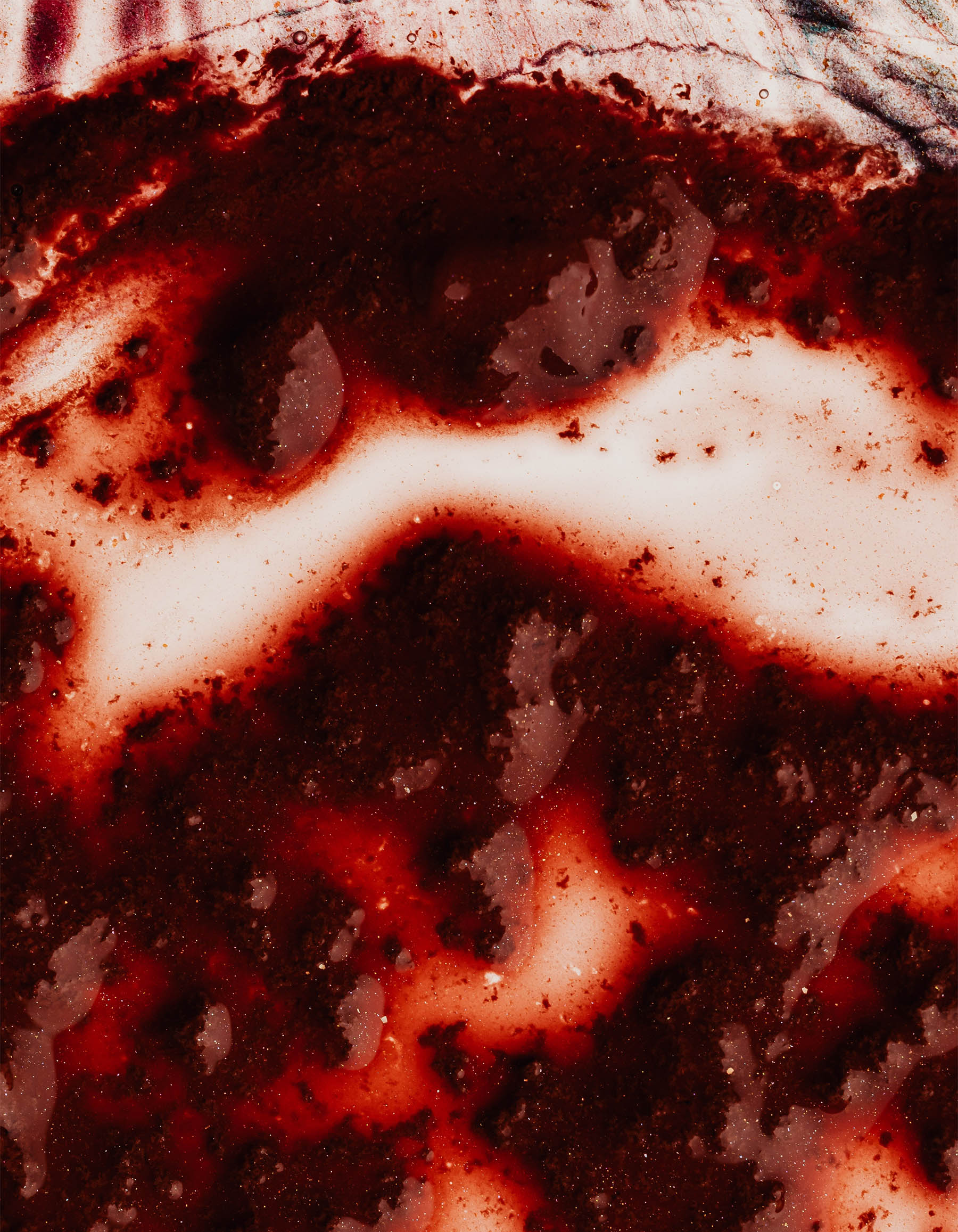
The most common sign of infertility is the inability to get pregnant after one year of regular, unprotected sexual intercourse, or six months if the woman is 35 or older. If you’re concerned about fertility, it’s helpful to recognize early signs, such as irregular menstrual cycles, very heavy or absent periods, persistent pelvic pain, or unexplained weight gain or loss. Paying attention to these signs, understanding risk factors, and consulting a healthcare provider can help you make informed decisions about your reproductive options.
We hope you’ll check out what they’re up to at https://modernfertility.com/flex. BTW, you can use that link to get an automatic $10 off your kit.
This article is informational only and is not offered as medical advice, nor does it substitute for a consultation with your physician. If you have any gynecological/medical concerns or conditions, please consult your physician.
© 2025 The Flex Company. All Rights Reserved.